This is the last of five steps in a series aimed at helping newly diagnosed people
understand some of the basics of a complex disease. The sequence of the first
four steps is DON'T
PANIC : GOOD NEWS! : DIAGNOSIS
: SURVIVING. If
you missed any of these first four steps, our recommendation is to go back and
follow them in sequence. Doing this will help you interpret some of the information
about the treatment choices. The
notion of choosing your own treatment for a medical problem is completely foreign
to most people. If you have a broken arm you expect it will be set in plaster;
if you have a child with acute appendicitis you expect they will have an appendectomy.
That is what the normal course of events is. There is no real discussion and often
no explanation. This is not the case with prostate cancer. There is a range of
options and these are set out below. It is in your own interest to research them
all. This page is followed by a page titled RESOURCES which summarizes some of
the sites, other than this one, where you might find additional useful information.
That page is linked from this page. CHOOSING
A TREATMENT THE
BASICS  The Golden Rule. The
Golden Rule of
prostate cancer is simple: THERE ARE NO RULES. This lack of rules creates
uncertainty. Uncertainty is difficult to deal with but is unavoidable.
The Golden Rule. The
Golden Rule of
prostate cancer is simple: THERE ARE NO RULES. This lack of rules creates
uncertainty. Uncertainty is difficult to deal with but is unavoidable.
 Every
Choice Has Consequences. No matter which choice is made, there are consequences.
Some are good, some less so. Much depends on the specific circumstances and few
are accurately predictable. Every
Choice Has Consequences. No matter which choice is made, there are consequences.
Some are good, some less so. Much depends on the specific circumstances and few
are accurately predictable.
 No
Good Data. There is a lack of really good information
about the outcomes and consequences of the treatment options. No one can guarantee
that what worked for one man will necessarily work for others. This makes it very
difficult to choose which path to follow. No
Good Data. There is a lack of really good information
about the outcomes and consequences of the treatment options. No one can guarantee
that what worked for one man will necessarily work for others. This makes it very
difficult to choose which path to follow.
 Status
Before Strategy. It is best to gather all possible information
about a diagnosis and all options available before making a choice. There are
many options; all should be considered. Status
Before Strategy. It is best to gather all possible information
about a diagnosis and all options available before making a choice. There are
many options; all should be considered.
 Choose
The Best Team: It may seem blindingly obvious,
but the skill and track record of the people chosen to advise, monitor and carry
out a procedure are the best predictors of a good result. There is an understandable
bias in the recommendation for treatment which must be recognized. For the same
diagnosis, surgeons will tend to recommend surgery; radiologists will tend to
recommend radiation. Choose
The Best Team: It may seem blindingly obvious,
but the skill and track record of the people chosen to advise, monitor and carry
out a procedure are the best predictors of a good result. There is an understandable
bias in the recommendation for treatment which must be recognized. For the same
diagnosis, surgeons will tend to recommend surgery; radiologists will tend to
recommend radiation.
CONSEQUENCES
OF CHOICES There
are consequences attached to all choices. Some are good consequences - the best
being there is no sign of the cancer after the procedure. Some are not so good
- these are usually referred to as side effects or morbidity. Impotence
[the inability to have an erection] and incontinence [the inability to control
your bladder or your bowel] are the ones that concern men the most. A brief summary
of potential consequences is
shown for
all the treatment options listed on this site. These are shown under the header
for each treatment choice together with the other relevant information. One of
the consequences that is frequently overlooked or not discussed is depression.
This subject is dealt with in this piece - DEPRESSION
- REAL OR INDUCED? It
is important to understand that the consequences of any choice are variable. There
are some actions that can reduce the potential severity of the negative consequences,
but sometimes a combination of the site of a tumor, the skill of a doctor or even
the attitude of the man undergoing the therapy can affect the outcome. It is also
often difficult to distinguish clearly between the consequences attached to the
choice made and the consequences of aging. What
data there is shows very little difference in outcomes and consequences for the
majority of men who have what is termed low risk or very low risk tumors, no matter
what path they choose. There are clear definitions of low risk or very low risk
tumors in the NCCN
GUIDELINES FOR PATIENTS - PROSTATE CANCER.
NO
GOOD DATA Most
men are surprised to find that there are no clear comparative guides as to outcome
of the various choices that might be available to them. There are many reasons
for this lack of data: some are more acceptable than others. But whatever the
reasons, the data is not there. To add to the confusion, new studies are published
frequently.
Some of these
seem to contradict other studies and some are interpreted by the media in ways
that ensure headlines rather than accuracy. This
lack of reliable, relevant data makes it extremely difficult to make an informed
decision as to which of the many treatment options is 'best' for you. Effective
Health Care published an excellent paper in February 2008 - Comparing the Effectiveness
of Therapies for Localized Prostate Cancer. The EXECUTIVE
SUMMARY (which runs to 20 pages and is in pdf format) is well worth
printing and studying. Some terms may be a little technical for the newly diagnosed,
but can be understood with a little work and by asking questions. A
paper entitled QUALITY
OF LIFE AND SATISFACTION WITH OUTCOME AMONG PROSTATE-CANCER SURVIVORS
was also published in 2008. The link above will get you to a copy of the paper.
It might also be worth reading the brief discussion on THE
"NEW" PROSTATE CANCER INFOLINK which highlights two points: "All
that the data from this study can do is offer you some general guidance about
what is reasonably expectable on average. The data are what they are. We wish
better guidance could be offered, but it just isn’t available." and "The
major takeaway from this study is that all forms of the most common types of treatment
have some downsides. The degree to which these may affect the individual patient
is the great unknown."
ON-GOING RESEARCH AND NEW DISCOVERIES
As if all this weren't confusing enough,
there is much research being done on new methods of cancer detection and treatment. Some of these methods involve nuclear medicine,
in which various amounts of specially-formulated radioactive isotopes are designed to seek out and attach themselves to very
specific types of cancerous prostate tissue and attack those malignant tissues on a cellular level, leaving normal cells unaffected.
One such study is the
Lutetium-177 PSMA radionuclide
therapy (Lu-PSMA) that is currently undergoing clinical studies in Australia (and other locations) for
advanced cases of Prostate Cancer that have spread to other parts of the body, when other treatment methods have already failed.
This new treatment method introduces a radioactive isotope molecule that specifically attaches to cells with high amounts of PSMA
("Prostate Specific Membrane Antigen"), which is a substance found in high levels on the surface of some prostate cancer cells.
The radioactive substance is injected in liquid form into the bloodstream and travels throughout the body, finding and attaching to the cancer cells
that the molecules were specifically designed to seek out and destroy. This allows the radiation to be delivered directly to the prostate
cancer cells wherever they have spread, while sparing most normal tissues. [Many thanks go to Stephen Taylor,
PhD at the University of New South Wales (Australia) and Principal Radiochemist at Liverpool Hospital in New South Wales, where he is one
of the key leaders in nuclear medicine research.]
New research and clinical trials continue
to expand our knowledge and the range of possible treatment methods, although it could be many years before these methods are proven to be safe and effective, and approved
for wide-spread use. Until that time, we must attempt to choose from among the treatment methods that are available today.
DEVELOPING A STRATEGY
Although
we recommend doing your own research into the choice you think will suit you best,
there are pitfalls. Although Steve Dunn was not diagnosed with prostate cancer
he has some excellent general advice in "CANCERGUIDE:
RESEARCHING YOUR OPTIONS". It may also help you understand
some of the issues that give rise to the uncertainty in the "the practice of medicine"
by reading INTERPRETING REPORTS,
a contribution from Dr Wesley Root. You
will find many apparently contradictory statements as you do your research. Much
of the confusion is due to the rivalry which exists between different branches
of the medical profession. For this reason it is important to try to establish
the background of anyone giving advice. In this way you may be able to detect
potential bias. Broadly speaking, urologists tend to recommend surgery, because
most of them are surgeons, while radiologists tend to recommend radiation therapy
for the same diagnosis. A paper published in 2010 titled IS
THERE AN OPTIMAL MANAGEMENT FOR LOCALIZED PROSTATE CANCER? (303KB
pdf file) sets out the state of play fairly well, although it does not mention
HIFU because that had not yet been approved by the FDA for use in the USA. Donna
Pogliano has some ADVICE TO THE
NEWLY DIAGNOSED. This piece of advice was written in 2004. There
have been some changes since then, notably the growth of RALP (Robotic Assisted
Laparoscopic Prostatectomy) aka Da Vinci procedures and a greater focus on Active
Surveillance. The basic advice is still relevant and sound. The piece is well
worth printing to keep and review as you develop your strategy. Donna was a prominent
prostate cancer activist and co-author of A
PRIMER ON PROSTATE CANCER, THE EMPOWERED PATIENT'S GUIDE.
Another
useful document showing a decision path is on the National Comprehensive Cancer
Network® (NCCN) site. You can download a copy of the
NCCN
GUIDELINES FOR PATIENTS - PROSTATE CANCER which
is supplied free of charge to registered users. (Registration is simple and there is no charge).
An article entitled "Comparative Analysis of PSA Free Survival Outcomes", by Dr. Peter Grimm et.al., was published in the British Journal of Urology International in 2012.
The original article provided a comprehensive comparison of eleven different treatment methods, but it was written for medical professionals, so it was very difficult for most people to understand.
Fortunately, the results were incorporated into a WEBSITE that presents the data in a graphical format that is relatively easy to understand.
Many educated layman will be able to understand the results with just a little help with the statistics. (Many thanks to YANA member and retired physician Dr. Brooke Jennings for finding this valuable resource.)
MAKING
YOUR CHOICE The
process of making a choice is a reiterative one. People will try to gain a good
initial understanding of all the options and their potential consequences before
rejecting some. They will then review the ones they have selected as potentially
being the best for them, both as far as their diagnosis and their personal outlook
on life. Through this process they should finally arrive at a decision that suits
them best. As
part of the process, it might be worthwhile to use the MCHUGH
DECISION SHEET and the MCHUGH
CHEAT SHEET to focus on what you want and what is best for you.
Dr John McHugh, the author of these documents is a urologist who was diagnosed
in 2007. If
you feel you need to know more there are two sources of information that you might
find helpful.  SURVIVOR
STORIES
on this site. More than one thousand men have contributed their experiences after
diagnosis with prostate cancer. Most of the men will respond to any specific questions
you might have. You can search the stories by a number of criteria to find a diagnosis
similar to yours. Telling your story on the site, even if you are still undecided
as to which choice you will make, will usually generate e-mail from some of the
veterans. If you want to do that come and JOIN
US.
SURVIVOR
STORIES
on this site. More than one thousand men have contributed their experiences after
diagnosis with prostate cancer. Most of the men will respond to any specific questions
you might have. You can search the stories by a number of criteria to find a diagnosis
similar to yours. Telling your story on the site, even if you are still undecided
as to which choice you will make, will usually generate e-mail from some of the
veterans. If you want to do that come and JOIN
US.
 The
YANA FORUM or one of the MAILING
LISTS. If you post there, setting out clearly the brief details
of your diagnosis, the treatment option you are interested in and what additional
information you need, you will almost certainly get a good response.
The
YANA FORUM or one of the MAILING
LISTS. If you post there, setting out clearly the brief details
of your diagnosis, the treatment option you are interested in and what additional
information you need, you will almost certainly get a good response.
Both
these sources of information are regarded with concern by some. It is felt that
using anecdotal information from non-medical people can lead to poor decisions.
However most people seem to understand the nature of the advice they get and where
it is coming from and find it useful as a platform to discuss with their medical
advisors. OPTIONS
The
most common options are listed below in alphabetical order from A through Z. Simply
click on the one you wish to learn about and you will be linked to the appropriate
place on the site. You may find that some treatments are known by more than one
name, so some links will take you to the same place. The
basic information for each of the options usually includes links to other sites
for more specific information. We have selected some that we think provide well
presented information. All websites listed within the YANA website are for information
purposes only - we do not endorse any particular website or organization. The
choice is with you as an individual, taking into account your specific requirements.
| ACTIVE
SURVEILLANCE : WATCHFUL
WAITING CONSERVATIVE
MANAGEMENT | The
tag of Conservative Management is rarely used now. Both Active Surveillance (AS)
and Watchful Waiting (WW) are used to describe the choice made by men who elect
not to have immediate conventional treatment. A distinction is often made between
the two:  Active
Surveillance (AS) involves undertaking a number of measures to track any changes
in a diagnosed early stage, low risk or very low risk disease. In the event that
there are significant changes, conventional treatment is undertaken with the intention
of effecting a cure. Active
Surveillance (AS) involves undertaking a number of measures to track any changes
in a diagnosed early stage, low risk or very low risk disease. In the event that
there are significant changes, conventional treatment is undertaken with the intention
of effecting a cure.
 Watchful
Waiting (WW) involves tracking changes and looking to manage any progress
of the disease without having initial invasive therapy. Watchful
Waiting (WW) involves tracking changes and looking to manage any progress
of the disease without having initial invasive therapy.
The
premise of both WW and AS is that most prostate cancers diagnosed today are slow
growing. If the cancer is early stage and low or very low risk there is a good
probability that the man in whom it is detected may die of another cause. Undertaking
conventional treatment with all the attendant negative consequences may be unnecessary
in such cases. Data from the PIVOT
STUDY published in July 2012 highlights this. There are two good
commentaries on the THE
"NEW" PROSTATE CANCER INFOLINK, the SECOND
OF WHICH concludes: -
For men with low-risk, early stage, localized prostate cancer who are older than
65 years of age and have a life expectancy of not more than 15 years, observation
(i.e., active monitoring) is now shown to be every bit as effective as (and a
great deal safer than) radical prostatectomy.
- For
men with low-risk, early stage, localized prostate cancer who are less than 65
years of age and have a life expectancy of more than 15 years, it is arguable
that observation (i.e., active monitoring) may be at least as good an option as
radical prostatectomy.
Neither
AS nor WW is regarded as a form of treatment in the sense that other therapies
set out to 'cure' the cancer. However, it may be a good option for some men who
have an appropriate diagnosis. Men most likely to have a suitable diagnosis for
this option are those who have what the Brady Institute at Johns Hopkins Memorial
Hospital has categorized as an "insignificant tumor", which they define
as set out below. There are other definitions of what is termed "low risk
cancer" which are similar:
- Nonpalpable - negative DRE (Digital Rectal Examination)
- Stage T1c
or T2a
- Percent free PSA 15 or greater
- Gleason 7a (3+4) or less
- Less
than three needle cores of twelve with none greater than 50% tumor
To provide health care providers, public health practitioners, policymakers, and
the general public with a comprehensive assessment of the current role of active
surveillance in the management of men with localized prostate cancer, the National
Cancer Institute, the Centers for Disease Control and Prevention, and the Office
of Medical Applications of Research convened a State-of-the-Science Conference
on December 5–7, 2011, to assess the available scientific evidence. Their report
ROLE OF ACTIVE SURVEILLANCE
IN THE MANAGEMENT OF MEN WITH LOCALIZED PROSTATE CANCER was published
in January 2012 and concluded: Active
surveillance has emerged as a viable option that should be offered to patients
with low-risk prostate cancer. More than 100,000 men a year diagnosed with prostate
cancer in the United States are candidates for this approach.
If you are considering this option it may be of interest to read these:  WATCHFUL
WAITING AND ACTIVE SURVEILLANCE: THE CURRENT POSITION,
published in July 2008 WATCHFUL
WAITING AND ACTIVE SURVEILLANCE: THE CURRENT POSITION,
published in July 2008
 ACTIVE
SURVEILLANCE FOR FAVORABLE RISK PROSTATE CANCER: What Are The Results, and How
Safe Is It?
A paper published in October 2010 ACTIVE
SURVEILLANCE FOR FAVORABLE RISK PROSTATE CANCER: What Are The Results, and How
Safe Is It?
A paper published in October 2010
 ACTIVE
SURVEILLANCE FOR PROSTATE CANCER: PATIENT SELECTION AND MANAGEMENT
is of interest, with one of the main points concerning the surveillance patients,
who were eventually treated. At a median follow up of about 8 years, absolutely
no difference was observed in the mortality or the metastasis rate. Most of the
men in the studies are still on AS. There is a post on the paper on the YANA
FORUM. ACTIVE
SURVEILLANCE FOR PROSTATE CANCER: PATIENT SELECTION AND MANAGEMENT
is of interest, with one of the main points concerning the surveillance patients,
who were eventually treated. At a median follow up of about 8 years, absolutely
no difference was observed in the mortality or the metastasis rate. Most of the
men in the studies are still on AS. There is a post on the paper on the YANA
FORUM.
 As
long ago as 1997 a lawyer who posted as Lorenzo Q Squarf wrote a series of amusing
(depending on your sense of humor) posts to a website and became involved in discussion
on the Internet about why Watchful Waiting was the best option for most men. His
website is no more - he went on his way, finding discussion of PCa 'boring' -
and was last heard of in 2011 at the ripe old age of 79 when, after he published
a book about his flying experiences, he provided a brief update. To get a taste
- and some intelligent thinking - on the subject of Watchful Waiting, part of
his website has been saved. It is here - FLAMEKEEPER
OF WESTERN CIVILIZATION.
As
long ago as 1997 a lawyer who posted as Lorenzo Q Squarf wrote a series of amusing
(depending on your sense of humor) posts to a website and became involved in discussion
on the Internet about why Watchful Waiting was the best option for most men. His
website is no more - he went on his way, finding discussion of PCa 'boring' -
and was last heard of in 2011 at the ripe old age of 79 when, after he published
a book about his flying experiences, he provided a brief update. To get a taste
- and some intelligent thinking - on the subject of Watchful Waiting, part of
his website has been saved. It is here - FLAMEKEEPER
OF WESTERN CIVILIZATION.
 The
question 'to treat or not to treat?' has been raised by many experts in the field,
including Dr Jonathan Oppenheimer, a leading pathologist in the US, who said this
in 2008: The
question 'to treat or not to treat?' has been raised by many experts in the field,
including Dr Jonathan Oppenheimer, a leading pathologist in the US, who said this
in 2008:
"For
the vast majority of men with a recent diagnosis of prostate cancer the most important
question is not what treatment is needed, but whether any treatment at all is
required. Active surveillance is the logical choice for most men (and the families
that love them) to make."  Positive
consequences of active surveillance:
Positive
consequences of active surveillance:
- The potential serious consequences of the conventional treatment choices
are avoided.
- There is a possibility of spontaneous regression. It is difficult
to even begin to estimate the probability of this occurring. However it is worth
noting that between 25% and 33% of men in AS studies do not have a second or subsequent
positive biopsy. This may be because of the "hit and miss" nature of
biopsy procedures. There is a discussion on SPONTANEOUS
REGRESSION on the Yana Forum which may be of interest. Dr Charles
"Snuffy" Myers discusses this issue on his site at DOES
CANCER EVER DISAPPEAR?.
 Negative
consequences of active surveillance:
Negative
consequences of active surveillance:
- The monitoring process chosen might not identify disease progression early
enough and late intervention may be less effective than early intervention.
-
There is a possibility of the initial diagnosis being incorrect because the diagnostic
tools used at present are not very accurate
.
- Most protocol for AS require repeat biopsy procedures which carry a small
degree of risk.
- Some of the problems associated with aging, such as an
increase in BPH (Benign Prostate Hyperplasia), may create urinary bothers such
as increasing frequency, nocturia and the like.
BACK
TO INDEX
| ANDROGEN
DEPRIVATION THERAPY(ADT) HORMONE
THERAPY : ANDROGEN BLOCKADE THERAPY |
This
therapy has many acronyms and names. Some examples are ADT, ADT2, ADT3, CAB, CHB,
CHB2, CHB3, CHT, HT, HBT. Technically all refer to the main object - to control
the body's production or absorption of testosterone (T) or, more precisely, dihydrotestosterone,
commonly referred to as DHT. Hormone therapy is sometimes described as a chemical
ORCHIDECTOMY - the advantage
is that it is reversible where surgical orchidectomy is not. A combination of
drugs may be used to prevent production of testosterone by the testicles and to
block the cancer tumor from using the testosterone produced by the adrenals. This
can reduce the size of the tumor in about 80% of cases. Historically,
hormone therapy was used mostly as a primary treatment of metastasized cancers
or as a salvage procedure for a failed treatment. The main measure of effectiveness
is the reduction in PSA levels. In some cases this is confirmed by the retreat
of metastasized lesions. It is also used as a primary treatment to reduce the
size of the prostate prior to other treatment - referred to as neo-adjuvant therapy
- and sometimes after primary treatment, such as radiation therapy, when it is
referred to as adjuvant therapy. Some surgeons will not operate on a prostate
where this therapy has been used prior to surgery as the treatment alters the
cellular structure of the gland itself. As
is the case with most issues to do with prostate cancer, there is considerable
disagreement about when and how this therapy should be applied. One area of considerable
disagreement has been the concept of interrupting the therapy when it appears
to have achieved a preliminary aim - the reduction in PSA levels. The therapy
is then resumed if and when PSA levels rise again. Some studies indicate that
such action may not be less effective than continuous therapy whilst producing
less negative consequences. An
excellent document has been produced recently (April 2012). It is entitled HORMONE
THERAPY FOR PROSTATE CANCER - A PATIENT GUIDE and it is well worth
reading. The
drugs used often have different names in different countries which can cause a
deal of confusion for the man trying to find information. It can be very useful
to use a search engine like Google to track these names. Some of the common names
of the drugs used to suppress the production of T (Testosterone) are: Lupron (leuprolide
acetate) and Trelstar (triptorelin pamoate) which are both injected intramuscularly
into the buttock. Zoladex (goserelin acetate) and Firmagon (degarelix acetate)
both injected subcutaneously into the lower abdomen. Viadur (leuprolide acetate)
which is surgically implanted into the upper arm. Although
leuprolide acetate is marketed as Viadur, Eligard, and Lupron in the USA, Lucrin
is the name used in countries like New Zealand, Australia, Belgium, Costa Rica,
Malaysia, Singapore and South Africa. In the UK and Ireland, leuprorelin is marketed
as Prostap SR (one-month injection) and Prostap 3 (three-month injection).  Positive consequences of ADT:
Positive consequences of ADT:
- When
used as a primary treatment of metastasized cancers or as a salvage procedure
for a failed treatment, the disease can be managed, sometimes for many years.
The popular delusion that this therapy will always fail within a year or two is
simply not correct.
- When
used as a neo-adjuvant or adjuvant therapy, there is some evidence that the outcome
of the primary therapy may be improved.
- There
is a growing body of evidence indicating that if this therapy is 'pulsed' or administered
on an intermittent basis, the negative consequences may be less severe without
affecting the ultimate outcome.
 Negative consequences of ADT:
Negative consequences of ADT:
- Reported
negative consequences of this therapy are numerous and are sometimes referred
to as ANDROGEN
DEPRIVATION SYNDROME, which results from lack of testosterone.
Some, but not all may be reversible if the treatment is stopped. Some of the frequently
identified negative consequences are listed below:
- The
principle negative consequence of major concern to men are loss of libido - the
desire for sexual activity - and erectile function - the ability to have an erection.
This therapy is often referred to as "chemical castration" and men can
be as eunuchs because of this. Although little can be done about the effects of
loss of libido and erectile function, whilst the drug is being administered this
piece - CASTRATED, EMASCULATED, BUT HARDLY
DISEMPOWERED! - might be useful for men concerned about emotional
aspects of these issues. There are links to useful sites dealing with erectile
dysfunction in the SURGERY
section.
-
Because there is a change in hormonal balance, emotions can change significantly,
with some men reporting depression and other emotional changes. Lack of clarity
of thinking and memory issues are also reported. A small pilot study published
in September 2012 titled "Cognitive problems in patients on androgen deprivation
therapy" is analyzed on THE
"NEW" PROSTATE CANCER INFOLINK.
- One
of the most serious negative consequences, especially where there is long term
use, is loss of bone mineral density or osteoporosis, which can result in fractures
and/or collapse of spinal vertebrae. This potential problem often gets less attention
than it should because it is less obvious until it may be too late.
- Less
serious, but very annoying is the development of what are termed in the USA as
hot flashes and as hot flushes in other version of English. There are no direct
health risks but these consequences may be relieved by using, with the approval
of your medical advisor, DEPO
PROVERA (medroxyprogesterone, a synthetic
form of the female hormone progesterone) or PAXIL
(paroxetine hydrochloride) or EFFEXOR
(venlafaxine hydrochloride).
- Other
general negative consequence are weight gain, fatigue or loss of energy, loss
of muscle mass, development of small breasts - medically termed GYNECOMASTIA,
loss of body hair and a general 'feminising' of the body. Although gynecomastia
is not uncommon in men who are not on this therapy, some men contemplating using
ADT will have a light radiation of the breast which, it is claimed, will reduce
the probability of this condition developing. As to muscle loss and fatigue, many
men have anecdotally reported that by increasing their exercise levels they have
been able to maintain their weight and energy levels and muscle mass.
- Many
men using ADT to manage their disease will develop what is termed CRPC (Castration-Resistant
Prostate Cancer) which is also known by many other terms, the most common being
AIPC (Androgen Independent Prostate Cancer) or HRD (Hormone Resistant Disease).
When this happens ADT is no longer effective and the man will need to consider
moving on to another therapy. This
has in the past meant CHEMOTHERAPY,
but there are other promising therapies being developed, the most well known at
present being PROVENGE.
The AUA American Urological Association released revised guidelines to the management
of men with CRPC in May 2013. You can read them here CASTRATION-RESISTANT
PROSTATE CANCER: AUA GUIDELINE
A
source of very detailed information on this subject is A Primer on Prostate
Cancer: The Empowered Patients Guide by Donnna Pogliano, a prostate cancer
activist. She co-authored the book with Dr Strum. It is not an 'easy read' to
glance through while lounging by the pool, but it allows laypeople to get a good
understanding of complex medical issues. The ISBN number is 0-9658777-6-0
and it has been available at Amazon and Barnes & Noble as well as at the LIFE
EXTENSION FOUNDATION site, whose support saw the book published. Long
term prostate cancer survivor CHUCK
MAACK (he was diagnosed in 1992 and has used ADT for many years
to manage his disease) has
collected information which he terms Observations, including some detailed aspects
of ADT on his own website THE PROSTATE ADVOCATE.
BACK
TO INDEX
| CASTRATION:
ORCHIDECTOMY/ORCHIECTOMY | The
orchidectomy or orchiectomy procedure is a surgical procedure where the testicles
are removed. This is done because it is an effective method of lowering the man's
testosterone level. Indeed it was the only way to create this effect before the
development of the drugs used more widely now. It is important to reduce the level
of testosterone as, in the current view, this is a major source of 'fuel' for
the growing prostate cancer. Although this procedure is still done, it
is usually only in countries where the cost of medication is unaffordably high.
It may also be suggested by some urologists if a man is diagnosed with advanced
prostate cancer late in his life. There is some technical information on the procedure
at WHAT
IS ORCHIECTOMY? A
similar effect can be produced through the use of ANDROGEN
DEPRIVATION THERAPY (ADT), which is reversible; an orchidectomy
is not.  Positive consequences of orchidectomy: The reduction of testosterone will
usually lead to a lowering of the PSA numbers and some alleviation of the symptoms
which men with advanced prostate cancer have.
Positive consequences of orchidectomy: The reduction of testosterone will
usually lead to a lowering of the PSA numbers and some alleviation of the symptoms
which men with advanced prostate cancer have.
 Negative consequences of orchidectomy: The main potentially negative consequences
are similar to those for ANDROGEN
DEPRIVATION THERAPY (ADT)
so are not repeated here. In addition there are often psychological issues. Prosthetic
implants inserted in the scrotum can help in this regard.
Negative consequences of orchidectomy: The main potentially negative consequences
are similar to those for ANDROGEN
DEPRIVATION THERAPY (ADT)
so are not repeated here. In addition there are often psychological issues. Prosthetic
implants inserted in the scrotum can help in this regard.
Ric
Masten was a poet. He had an orchidectomy. For his view of his procedure, read
his poem BILATERAL ORCHIDECTOMY
BACK
TO INDEX
It
would be very unusual for chemotherapy to be used as a primary therapy for early
stage prostate cancer, the most commonly diagnosed form of the disease. It's main
use is in connection with late stage disease, either on diagnosis - a small number
of cases these days - or where the primary therapies have failed and where hormone
refractory cancer has developed. This is commonly termed HRPC or androgen independent
prostate cancer (AIPC), although there are other terms. This hormone
refractory stage is where ANDROGEN
DEPRIVATION THERAPY (ADT) is no longer effective. In most cases
where chemotherapy is used there will be evidence of metastasized disease. Historically
studies showed that chemotherapy was not a very effective treatment for prostate
cancer and there were very serious negative consequences from the large doses
of toxic chemicals used. In
recent years, use of chemotherapy for prostate cancer has changed significantly
and smaller, intermittent doses are now used. This has resulted in less negative
consequences and seems to provide a better tool to manage the disease.
There are no claims that chemotherapy can 'cure' prostate cancer, but there is
a growing body of evidence that shows that the disease can be managed for some
time using modern drugs.
There is an excellent summary of the 'state of play' at June 2010 in this piece
THE
CONVERSATION BEHIND THE SCENES AT ASCO on The "New" Prostate
Cancer Infolink. Some of the therapies mentioned in this piece have subsequently
been approved and are in general use. A very useful site that offers the general
information on chemotherapy for cancer patients and their families, caregivers
and friends is Scott Hamilton's site CARE
DURING CHEMOTHERAPY AND BEYOND A useful paper, mainly aimed at
people diagnosed with esophageal cancer, but providing good insight into nutrition
during chemotherapy is THE
FULL SPECTRUM  Positive consequences of chemotherapy:
Positive consequences of chemotherapy:
- Many
of the studies show what might be considered relatively short extension of life
expectancy. For example the difference in survival in the well publicized PROVENGE
study was only four months. However this is in the comparison of median
survival periods and, as this piece THE
MEDIAN ISN'T THE MESSAGE demonstrates so clearly, it is the range
of survival times that is more important than the median. One well known oncologist
claims that modern chemotherapy means that the majority of men treated will live
out their normal life span. In considering this statement it should be borne in
mind that many men treated with chemotherapy are old or sickly and may not have
a long normal life span.
 Negative consequences of chemotherapy:
Negative consequences of chemotherapy:
-
There is a wide spectrum of negative consequences although these are less severe
than those encountered historically. They may still impact severely on men who
are not well when they start the therapy. The loss of hair is less common than
it was and even the intense nausea that was inevitable is less so. One such drug,
Taxotere, has had multiple reports of ADVERSE SIDE EFFECTS.
BACK
TO INDEX
| COMPLEMENTARY
AND ALTERNATIVE MEDICINE THERAPIES (CAM) | There
are many definitions of Alternative Medicine. Probably the most widely used -
in the USA in any event - is 'medical interventions not taught at United States
medical schools or not available at United States hospitals.' A more international
definition might be 'an unrelated group of non-orthodox therapeutic practices,
often with explanatory systems that do not follow conventional biomedical explanations.'
These
practices are often referred to as 'quackery', yet indications are that an ever-increasing
number of people in the USA and Europe are resorting to them. Sometimes they are
used alone as an alternative to conventional treatment; sometimes they are used
as a complement, to help conventional treatment. There
are many claims made for alternative medicine that do not stand up to scrutiny
and so it is important to be aware of this before accepting professed claims from
people who are making money from their claims. There are three basic questions
that should be answered - and they may also apply to conventional medicine.
- Is there any independent evidence to support the claims being made?
- Will
the person providing the information benefit directly or indirectly from what
they are claiming?
- How long is it since the evidence supporting the claim
was collected or completed?
An
example of this approach is in the JANUARY
2012 YANA-E LETTER under the header Will this work?  Steve Dunn gives a good preliminary view on the value of Alternative Medicine
on his site at STEVE
DUNN'S CANCERGUIDE MATERIAL ON ALTERNATIVE THERAPIES. If you do
go there, be sure to also read the two sections of the site - ALTERNATIVE
THERAPIES: HOPE OR HYPE? and SEPARATING
THE WHEAT FROM THE CHAFF
Steve Dunn gives a good preliminary view on the value of Alternative Medicine
on his site at STEVE
DUNN'S CANCERGUIDE MATERIAL ON ALTERNATIVE THERAPIES. If you do
go there, be sure to also read the two sections of the site - ALTERNATIVE
THERAPIES: HOPE OR HYPE? and SEPARATING
THE WHEAT FROM THE CHAFF
 For a widely-praised example of what the medical profession thinks we should all
be aware of - go to QUACKWATCH.
Check the index for any specific treatment or therapy, but be aware that some
of the entries may not meet the three criteria set out above.
For a widely-praised example of what the medical profession thinks we should all
be aware of - go to QUACKWATCH.
Check the index for any specific treatment or therapy, but be aware that some
of the entries may not meet the three criteria set out above.
 The ANNIE
APPLESEED PROJECT provides information, education, advocacy, and
awareness for people with cancer and their family and friends. There is a very
broad range of information which will be helpful in evaluating alternative options.
The MEMORIAL
SLOAN-KETTERING CANCER CENTER (MSKCC) web site has a database on
use of hundreds of vitamins, herbal agents, botanicals, and supplements. This
database has been developed by the Department of Integrative Medicine at MSKCC. The ANNIE
APPLESEED PROJECT provides information, education, advocacy, and
awareness for people with cancer and their family and friends. There is a very
broad range of information which will be helpful in evaluating alternative options.
The MEMORIAL
SLOAN-KETTERING CANCER CENTER (MSKCC) web site has a database on
use of hundreds of vitamins, herbal agents, botanicals, and supplements. This
database has been developed by the Department of Integrative Medicine at MSKCC.  Smilow Comprehensive Prostate Cancer Center claims that they have a specialty
focussing on HOLISTIC
TREATMENT OF PROSTATE CANCER. The principles of their approach
show nothing that is really new. However they are one of a small number of institutions
providing an integrated series of therapies.
Smilow Comprehensive Prostate Cancer Center claims that they have a specialty
focussing on HOLISTIC
TREATMENT OF PROSTATE CANCER. The principles of their approach
show nothing that is really new. However they are one of a small number of institutions
providing an integrated series of therapies.
 There is also an excellent book dealing with the subject: CHOICES
IN HEALING by Michael Lerner. (This
book can be read online free of charge - it is highly recommended reading, with
a suggestion that reading the last chapter first, may provide some comfort and
insight).
There is also an excellent book dealing with the subject: CHOICES
IN HEALING by Michael Lerner. (This
book can be read online free of charge - it is highly recommended reading, with
a suggestion that reading the last chapter first, may provide some comfort and
insight).
 Nelson Berman has written an account of his decision to take the Alternative route
- his site is at CANCER
IS NOT THE ENEMY.
Nelson Berman has written an account of his decision to take the Alternative route
- his site is at CANCER
IS NOT THE ENEMY.
 PC-SPES AND PROSTASOL
are probably the best known alternative therapies. PC-Spes is no longer available
but there are many compounds making similar claims for efficacy. The best known
is Prostasol.
PC-SPES AND PROSTASOL
are probably the best known alternative therapies. PC-Spes is no longer available
but there are many compounds making similar claims for efficacy. The best known
is Prostasol.
 SALVESTROLS It seems that
there may be a focus developing on this compound, developed by Dr Gerry Potter,
credited with the original research which led to the development of ZYTIGA.
SALVESTROLS It seems that
there may be a focus developing on this compound, developed by Dr Gerry Potter,
credited with the original research which led to the development of ZYTIGA.
 Positive consequences of CAM:
Positive consequences of CAM:
- Some complementary and alternative medicine therapies may well improve
overall health. This may then enhance the immune system to such an extent that
the cancer is sent into regression.
- The consequences of conventional therapies
may be lessened or managed better by using complementary and alternative medicine
therapies.
 Negative consequences of CAM:
Negative consequences of CAM:
- Some complementary and alternative medicine therapies may clash with conventional
medication. For this reason, the use of such therapies should always be discussed
with medical advisors before commencing the therapy.
- Very few complementary
and alternative medicine therapies have clear evidence for their efficacy in managing
prostate cancer. Relying on such therapies can result in the disease advancing
to a stage where any prospect of cure by conventional means is lost.
BACK
TO INDEX
In
recent years there has been renewed interest in using cryotherapy for localized
prostate cancer. This therapy destroys prostate tissue (both cancerous and normal
cells) by freezing the prostate gland with liquid argon which is delivered through
thin needle-like probes. The
probes are placed through the perineal skin - between the scrotum and anus. They
are guided using transrectal ultrasound which is also used to monitor the freezing
process in real time. The number of probes will vary depending on the size of
the prostate and the position and size of any specific tumor sites. Liquid argon
gas is used to reduce the temperature very rapidly. Although
this treatment is referred to as being effective because of the freezing of the
gland and thus destroying the tissue, it is, in fact, the very rapid thawing process
which ruptures the cell membranes effectively killing the cells. The freezing/thawing
cycles is usually carried out in two or three cycles. A catheter is inserted in
the urethra, which carries urine from the bladder to the penis, and warm liquid
is circulated during the procedure to stop the freezing of cells in the urethra
to limit any urinary problems. When
this procedure was first used, the entire gland was destroyed resulting in a high
rate of erectile dysfunction (ED) - almost 100% of men were impotent according
to some studies. Later refinements have seen a more targeted approach, which aims
at destroying only identified tumors and the healthy cells in the immediate vicinity
of the tumor. This can leave some or all of the erectile nerves untouched and
results in levels of ED that are comparable with those resulting from other treatments.
This is usually referred to as FOCAL THERAPY.
One advantage this form of treatment is that it can be repeated. It can also be
used as a salvage procedure for other failed treatments, notably radiation treatment
- EBRT (External Beam Radiation Treatment) or Brachytherapy.  This CRYOTHERAPY
site is a very useful one for anyone considering this option.
This CRYOTHERAPY
site is a very useful one for anyone considering this option.
 One of our Mentors, the late COLIN
CAMPBELL wrote a piece "WHY
CRYOSURGERY" that may be of interest.
One of our Mentors, the late COLIN
CAMPBELL wrote a piece "WHY
CRYOSURGERY" that may be of interest.
 Gary Onik is a pioneer of this therapy. FOCAL
NERVE SPARING FOR CRYOTHERAPY (a downloadable pdf) was published
in 2002 and describes a pilot study. A later paper published in 2005 is available
at HEALTHY
AGING or may be accessed as THE
MALE LUMPECTOMY - a printable Word.doc
Gary Onik is a pioneer of this therapy. FOCAL
NERVE SPARING FOR CRYOTHERAPY (a downloadable pdf) was published
in 2002 and describes a pilot study. A later paper published in 2005 is available
at HEALTHY
AGING or may be accessed as THE
MALE LUMPECTOMY - a printable Word.doc
 Men considering this option might find it helpful to review STUFF
TO TAKE WHEN EXPERIENCING CRYOSURGERY, written by a man who underwent
this therapy and wanted to share his experience.
Men considering this option might find it helpful to review STUFF
TO TAKE WHEN EXPERIENCING CRYOSURGERY, written by a man who underwent
this therapy and wanted to share his experience.
 Positive consequences of cryotherapy:
Positive consequences of cryotherapy:
- Although there are no good, long term studies to determine the efficacy
of cryotherapy, published data indicates similar 'cure rates' to other therapies
for low risk or very low risk diagnoses. It is unusual for cryotherapy to be used
for high risk diagnoses. Effectiveness is measured by taking PSA tests. Typically
it may take about three months for PSA numbers to reach their nadir - their lowest
level.
- Cryotherapy can be used as a salvage therapy in the event of failure
of initial therapy.
 Negative consequences of cryotherapy:
Negative consequences of cryotherapy:
Short
Term:
- The entry of needles in the perineum can cause irritation, swelling and
inflammation in this and the genital areas. This usually responds to icing and
anti-inflammatory drugs.
- Fluid can also collect in the scrotum, although
this is more rare. Medical help should be sought.
- There may be some itching
and burning during urination in the immediate aftermath of the treatment as well
as some urgency and blood in the urine. These consequences usually dissipate over
a few days. If they do not, medical help should be sought.
- Damage may
occur to the urethra, despite the precautions taken to keep this area warm. This
damage may lead to what is termed urethral sloughing - the passage of dead tissue
through the urethra. In severe cases there will be urinary obstruction requiring
medical treatment - usually catheterisation initially. Men who have undergone
transurethral resection of the prostate (TURP) or using cryotherapy as a salvage
treatment are at higher risk for urethral sloughing.
Long
Term:
- Although the incidence of Erectile Dysfunction (ED) - the inability to
have an erection - is reportedly similar to other therapies where a focal therapy
is carried out, full cryotherapy usually results in loss of erectile function
- The
development of a fistula is one of the more serious consequences of cryotherapy.
The numbers of fistula occurring has been reduced with modern technologies. In
the worst cases, a channel forms between the urethra and the rectum. This allows
matter - urine and fecal matter - to pass from one part of the body into another.
The results can include diarrhea, rectal incontinence or urinary tract infections.
- Most
urinary problems that might arise are likely to be short term as listed above.
BACK
TO INDEX
One
of the significant advances in the treatment of breast cancer was the development
of the so called "lumpectomy". This procedure sees the removal of only the material
identified as cancerous instead of the entire breast - the mastectomy, which was
standard practice. The lumpectomy can only be done in suitable cases where the
disease is diagnosed at an early stage. It is claimed that there is a similar
success rate to mastectomy procedures in such cases. The
question inevitably arose as to whether a similar process could be applied to
early stage prostate cancer. To date there is no surgical procedure which will
only remove a part of the prostate gland, but there are some therapies for which
it is claimed that only the diseased part of the gland will be ablated (destroyed)
by the treatment. The main therapies for which this claim is made to date are
CRYOTHERAPY, HIGH INTENSITY
FOCUSSED ULTRASOUND (HIFU), PHOTODYNAMIC
THERAPY (PDT), IRREVERSIBLE
ELECTROPORATION (IRE) and LASER
FOCAL THERAPY. Some of these are at the time of writing (March
2013) regarded as experimental and some are known by other terms. Detailed information
as to how they are applied and the potential consequences are detailed in the
relevant sections dealing with these therapies where such information is available.
One
of the main issues when considering whether to have a focal therapy, with its
promise of potentially reduced negative consequences, is how to identify just
which part of the gland is to be treated and which is to be preserved. There are
essentially two options neither of which is entirely satisfactory because of the
heterogeneous nature of prostate cancer which commonly is multi-focussed. There
is a very real possibility of some cancerous material being missed and therefore
not treated.  Scans used at present are far from accurate, producing both false positive
and false negative results. That is to say they sometimes miss tumors and at other
times signal that there are tumors where none exist. There is some evidence that
the use of what are termed COLOR
DOPPLER scans may increase the probability of tumors being identified.
Scans used at present are far from accurate, producing both false positive
and false negative results. That is to say they sometimes miss tumors and at other
times signal that there are tumors where none exist. There is some evidence that
the use of what are termed COLOR
DOPPLER scans may increase the probability of tumors being identified.
 Biopsy: A more common approach in trying to identify the presence of tumors
is to undertake what is usually termed as a saturation biopsy procedure. Other
terms are also used for this procedure. Where a normal biopsy procedure will use
twelve needles to take samples, the saturation biopsy will use upwards of thirty
needles, the precise number depending on the estimate size of the prostate gland.
This procedure is carried out under anesthesia and entry is through the perineum
- the area between anus and scrotum. The multiple results are then plotted on
a grid to identify any diseased areas.
Biopsy: A more common approach in trying to identify the presence of tumors
is to undertake what is usually termed as a saturation biopsy procedure. Other
terms are also used for this procedure. Where a normal biopsy procedure will use
twelve needles to take samples, the saturation biopsy will use upwards of thirty
needles, the precise number depending on the estimate size of the prostate gland.
This procedure is carried out under anesthesia and entry is through the perineum
- the area between anus and scrotum. The multiple results are then plotted on
a grid to identify any diseased areas.
A
good paper published by PCRI in 2010 REVIEW
OF FOCAL THERAPY FOR LOCALIZED PROSTATE CANCER summarizes the position
well.  Positive consequences of focal therapies:
Positive consequences of focal therapies:
- If the focal therapy is accurately guided to ablate only diseased tissue,
there is a significant reduction in the potential for negative consequences.
- If
the focal therapy fails initially it can be repeated, aimed at any new area identified
as being missed on the first treatment.
- The limited number of studies
on focal therapies show that they are most successful with low risk or very low
risk diagnoses. There are no long term studies of focal therapies.
 Negative consequences of focal therapies:
Negative consequences of focal therapies:
- Although an accurately guided focal therapy procedure will reduce the
probability of negative consequences significantly, the consequences associated
with the relevant 'non-focal' therapies are still possible.
- In trying
to minimze the negative consequences of the focal therapy, some small clusters
of cells may be missed and not treated.
BACK
TO INDEX
| HIGH
INTENSITY FOCUSED ULTRASOUND (HIFU) | HIFU
is a FOCAL THERAPY. Ultrasound
waves are focused on targeted areas of the prostate which are heated to temperatures
of 80 to 100 °C , very much higher than the normal body temperature of 37°C. This
kills the tissue on which they are focused. In effect HIFU is the precise reverse
of CRYOTHERAPY. One freezes the
prostate cancer to death, the other cooks it to death.
HIFU is an FDA-approved minimally-invasive alternative to prostate tissue ablation (destruction).
HIFU uses ultrasound energy to generate heat that ablates targeted tissue within the body. Focused
sound waves that are generated by a transducer pass safely through tissue until they reach the focal point,
where they produce enough heat to destroy tissue. With this technology, physicians can
customize each individual procedure, targeting as little or as much tissue as needed, and adjusting the
ablation during its course such that the identified target volume is destroyed fully. This also allows for
preservation of healthy tissue within the prostate, eliminating the need to remove the entire gland.
The ability to customize the ablation while it is being delivered, and to avoid critical structures, helps maintain quality of life and
preserve urinary continence and erectile function.
A HIFU procedure lasts about 2-4 hours and is usually performed under general anesthesia. A probe is
inserted into the rectum and HIFU energy safely passes through the rectal wall to destroy prostate tissue.
Post procedure, patients may need a catheter to help with urination, which can stay in place for 1-2
weeks. Patients can expect to be in the recovery room for about 2-4 hours and often return to mild
activities later that same day.
Much
of the information about HIFU is supplied by the two major manufacturers ABLATHERM®
and SONABLATE® 500
and should be viewed in that light. A paper published in 2005,
TRANSRECTAL
HIFU: THE NEXT GENERATION?, highlights some of the significant
differences between the two manufacturers' equipment and operation.
Although this procedure has been used for several years in
Europe, it was only recently approved for use in the United States. One manufacturer claimed in
2009, ten years after development of their prototype machine, that more than 15,000
men had been treated with their equipment at about 180 centers around the world
- mainly in Europe. At September 2010 HIFU had been approved for use in Australia,
Bahamas, Bermuda, Britain, Canada, China, France, Germany, Japan, Korea, Mexico
and Puerto Rica. In the United States, the Food & Drug Administration (FDA)
approved the SONABLATE® 450
device for use in treating Prostate Cancer in October of
2015. Previously, many men in the US traveled to nearby countries for the procedure.
The National Institute for Health and Clinical Excellence (NICE) has issued
FULL
GUIDANCE to the use of HIFU which may be of interest to anyone
contemplating the use of this therapy. It was reported in March 2013 that documentation
had been submitted to the U.S. Food & Drug Administration (FDA) for pre-market
approval of the Ablatherm device - EDAP
TMS SUBMITS DATA FOR APPROVAL OF HIFU TO US FDA.
There
are few independent published studies. These are commentaries on some of those
published since 2009 with links to Abstracts of the original studies which are,
of necessity, not based on US data:  UK study 2009: CONTROVERSY
IN THE APPROPRIATE USE OF HIFU
UK study 2009: CONTROVERSY
IN THE APPROPRIATE USE OF HIFU
 French study 2010: HIFU
IS NOT NECESSARILY AS SAFE AS SUGGESTED
French study 2010: HIFU
IS NOT NECESSARILY AS SAFE AS SUGGESTED
 German study 2010: BLADDER
OUTLET OBSTRUCTION: A COMMON SIDE EFFECT OF HIFU
German study 2010: BLADDER
OUTLET OBSTRUCTION: A COMMON SIDE EFFECT OF HIFU
 Korean study 2012 : HIFU
"DOES NOT PROVIDE EFFECTIVE ONCOLOGIC OUTCOMES"
Korean study 2012 : HIFU
"DOES NOT PROVIDE EFFECTIVE ONCOLOGIC OUTCOMES"
 Small initial short term UK trial 2012: FOCAL
HIFU IN MEN WITH LOCALIZED PROSTATE CANCER
Small initial short term UK trial 2012: FOCAL
HIFU IN MEN WITH LOCALIZED PROSTATE CANCER
 Canadian men treated with HIFU 2012: 4-YEAR
BIOCHEMICAL PROGRESSION-FREE SURVIVAL (bPFS)
Canadian men treated with HIFU 2012: 4-YEAR
BIOCHEMICAL PROGRESSION-FREE SURVIVAL (bPFS)
 Regensburg in Germany HIFU data 2013: HIFU
OUTCOMES IN GERMANY AFTER 8 YEARS OF FOLLOW-UP
Regensburg in Germany HIFU data 2013: HIFU
OUTCOMES IN GERMANY AFTER 8 YEARS OF FOLLOW-UP
Specialists
who can carry out the HIFU procedure in countries adjacent to the US are listed
in HIFU - PHYSICIANS
AND DOCTORS DIRECTORY. At
March 2013, the site had not been updated for eighteen months. It
seems that this site might replace a previous site which was the subject of this
commentary: WHY
YOU SHOULDN'T BELIEVE EVERYTHING YOU READ. Another
form of heat treatment for prostate cancer has been termed "hypertherapy".
This is the speciality of a German clinic and their claim is that by heating the
prostate gland cancer cells are killed while healthy cells remain untouched. This
appears to be a form of hyperthermia. Hyperthermia has been used for many years,
usually in conjunction with other therapies such as EBRT (External Beam Radiation
Therapy) or Chemotherapy. Some information is on the BICHER
CANCER INSTITUTE site. Although claims are made that this procedure
can be used successfully for prostate cancer, there are no specific studies that
demonstrate this. The studies listed on the site appear to have Dr Bicher as the
author.  Positive consequences of HIFU:
Positive consequences of HIFU:
- There is no invasive surgery. The beam of ultrasound rays is delivered
transrectally into the prostate, through the rectal wall closest to the prostate.
- Ultrasound
is not an ionizing form of radiation (which radiotherapy is). Therefore tissue
along the entry path and the exit path of the ultrasound beam may be less likely
to be significantly affected.
- It is a single treatment, like seed implants
- BRACHYTHERAPY. One day —
in and out (at least in theory).
- It is a repeatable treatment. In other
words, if the first round of treatment fails to deal with the tumor it is possible
to have a second treatment.
 Negative consequences of HIFU:
Negative consequences of HIFU:
- There is no doubt that there have been serious consequences associated
with HIFU, the worst of which result in painful rectal fistula and bladder obstruction.
It is claimed that these poor consequences are associated with early procedures
or poorly trained operators.
- It is possible that the long term 'cure rates'
may not be as good as other therapies and that there may be long term negative
consequences. There are no studies in this connection.
BACK
TO INDEX
| IRREVERSIBLE
ELECTROPORATION (IRE) NANOKNIFE |
In
recognition of the negative consequences of the most common treatments, there
has been a number of efforts to develop what are termed FOCAL
THERAPIES. One such development is termed Irreversible Electroporation
(IRE) which is also known as Nanoknife It is far from clear why, apart from marketing
implications of 'something new' the term 'nano' was introduced, since there is
no nano technology apparent in the material published to date. It
is claimed that IRE uses short pulses of direct electric current to create irreversible
damage to cancer cell membrane thus causing cell death. It is also claimed that
any other cells damaged in the process will regenerate, although it is far from
clear why cancer cells will not also regenerate. The electrodes that provide the
pulses of electric current are placed in pairs on each side of the target material.
This creates the same problem for IRE as it does for other focal therapies - the
inability to identify precisely all the material that is to be ablated. A paper
authored by leading researcher Dr Gary Onik, IRREVERSIBLE
ELECTROPORATION: IMPLICATIONS FOR PROSTATE ABLATION, sets out the
procedure. Some of the detail seems to clash with that in the German site, translated
as GENTLE
TREATMENT OF PROSTATE CANCER. This proposed
therapy is without a doubt classified as experimental. BACK
TO INDEX
In
recognition of the negative consequences of the most common treatments, there
has been a number of efforts to develop what are termed FOCAL
THERAPIES. One study for which a completed
formal Phase I trial was completed in 2013 used MRI guided laser beams generated
by a device inserted through the perineum into the prostate gland. The
use of heat to attack the cancer cells is the same concept as that used in HIFU
but the delivery system is very different. A small catheter is inserted and used
it to guide a tiny optical fiber, the laser and a cooling device into the prostate.
Under MRI guidance, the laser is positioned within the cancer and used to heat
the area to a temperature that would kill cancer cells. Temperatures outside the
treatment region are checked to protect healthy tissue, especially those near
critical structures such as the urethra and rectal wall. The
Media Release regarding the initial study is titled FOCAL
THERAPY OFFERS MIDDLE GROUND FOR SOME PROSTATE CANCER PATIENTS
and there is a good commentary on the paper at DATA
FROM A FORMAL PHASE I TRIAL OF MR-GUIDED, FOCAL LASER SURGERY This
proposed therapy is without a doubt classified as experimental. BACK
TO INDEX
PC-Spes
(Spes is the Latin word for Hope) was regarded as an alternative treatment that
worked and there were many reports of excellent results. At least one study was
being undertaken and the early report were promising that this might be, as was
claimed, a herbal recipe that could cure prostate cancer, at least as demonstrated
by the control of PSA results. Concerns
were raised however that the compound might rely on estrogen compounds and that
these might give rise to thrombosis. The compound did not have FDA approval and
was heavily criticized in The New England Journal of Medicine -- September 17,
1998 issue. It was withdrawn from the market following action by the government
of California and was the subject of considerable litigation. There are other
clones such as PC-HOPE,
PC-CARE and PC-PLUS which are claimed to be as effective as PC-Spes,
although none appear to be so, based on anecdotal evidence. The article linked
above concludes with this stern warning: "Using
these herbal products instead of conventional treatments for prostate cancer could
be very harmful to your health."
One
of the best known clones is a compound marketed as PROSTASOL.
There are said to be two versions of this - Dr Donsbach's which is apparently
made in Mexico and marketed mainly in the USA and another marketed in Europe.
The precise compound of Prostasol is unknown, the contents are not stated on the
packaging and may change from time to time. It also appears that there may be
significant differences between the Mexican and European versions. The DANISH
MEDICINE AGENCY WARNING published in 2007 states in part: "The
description of the contents states that Prostasol is a pure herbal product, but
a Danish analysis shows that Prostasol contains diethylstilbestrol (synthetic
estrogen)." There have been reports of men suffering from thrombosis
- see PROSTASOL
AND VENOUS THROMBOEMBOLISM as an example - and great care should
be taken in using these compounds, which should only be taken under medical supervision.
It may be necessary to use warfarin/coumadin to reduce the potential for blood
clotting. DR
DONSBACH was arrested in April 2009, and charged with 11 felony
counts including treating patients without a license, misbranding drugs for sale,
grand theft, unlawfully dispensing drugs as a cure for cancer, and falsely representing
a cure for cancer. When the case came to trial in 2010 Donsbach pleaded guilty
to thirteen felonies: five counts of practicing medicine without a license, five
counts of selling/distributing misbranded drugs, and one count each of attempted
grand theft, grand theft, and being a felon in possession of a firearm. The
reference to a previous felony was to a crime for which Donsbach was sentenced
to a year in jail, although he did not serve this time. He also admitted that
he personally inflicted a great bodily injury on one of the victims related to
the unlicensed practice of medicine. The Court agreed to sentence Donsbach to
probation, which will include restrictions against practicing medicine and distributing
dietary supplements, and possible custody in the county jail. BACK
TO INDEX
| PHOTO
DYNAMIC THERAPY (PDT) |
PHOTODYNAMIC THERAPY(PDT)
has been used to treat cancer for more than 25 years. Although the focus has been
primarily on surface or superficial lesions, such as skin cancer, there has been
a movement to find ways of treating deeper malignancies, such as prostate cancer.
The way in which this therapy works is that a photosensitizing drug is introduced.
When this is irradiated by light at a specific wavelength it generates cell death,
primarily through apoptosis, micro vascular damage, and an anti-tumor immune response.
In treating prostate cancer infrared light is introduced to the gland by probes
inserted through the perineum in much the same way as Brachytherapy probes. The
procedure has not been approved by the FDA for the treatment of prostate cancer.
There is a growing body of evidence concerning its efficacy and the innate minimally
invasive characteristics of PDT suggest that it should become an important addition
to the growing array of techniques in interventional oncology, provided that the
issues raised in FOCAL THERAPIES
are resolved. An
excellent piece published in Nature Clinical Practice Urology in early 2009 is
PHOTODYNAMIC
THERAPY FOR PROSTATE CANCER-A REVIEW OF CURRENT STATUS AND FUTURE PROMISE.
It is a fairly technical article but this paragraph extracted from the article
sums up the conclusions : The
benefits of prostate cancer treatment depend upon eradication of cancer within
the gland, while the harms of treatment are related to unwanted effects outside
the gland. When treatment is limited to either the prostate gland itself, or the
areas of cancer within the gland where possible, then there is the potential to
achieve the survival benefits of radical treatments in those men who require it,
while avoiding the associated adverse effects. Such an approach would have to
eradicate clinically relevant cancer, while at the same time leave the structures
that surround the prostate (including the rhabdosphincter, rectum, neurovascular
bundles and ejaculatory apparatus) intact. Eventually, a systemic but targeted
therapy will likely meet these requirements; however, as no obvious compound with
these attributes is currently in clinical studies, it is fair to assume that we
are at least a decade away from such a treatment becoming a reality. BACK
TO INDEX
Provenge
- Sipuleucel-T (APC8015) - is manufactured by Dendreon Corporation, and is referred
to as a therapeutic cancer vaccine for prostate cancer. This is an unusual term
for those who think of a vaccine in terms of a preventive vaccine, which prevents
infectious disease. Provenge does not do that. In practical terms Provenge operates
as an immunostimulant. The therapy is a complex one to administer and has to be
prepared specifically for each patient. Because of this it is expensive, being
marketed initially at a cost of $93,000.
The
first step is a process known as leukapheresis which separates out white blood
cells - primarily dendritic cells - which are required for the therapy and and
which then returns the remaining blood to the circulation. This process takes
about three hours during which the man has to remain still and in a supine position.
The
cells that have been removed from the blood are then processed by Dendreon . The
process prepares the dendritic cells for targeting the antigen prostatic acid
phosphatase (PAP) which is said to be present in 95% of PCA cells and boosts their
immune signaling factors.
The
activated blood product is returned to the infusion center and re-infused into
the patient with the aim of causing an immune response against cancer cells carrying
the PAP antigen.
A
complete Provenge treatment requires three collection/reinfusion procedures over
the span of a month, with two weeks between successive procedures.
There
has been a great deal of controversy regarding Dendreon and the development for
Provenge for many years. There have been allegations of conflicts of interest
among two members of an FDA advisory panel, stock price manipulation and patent
protests over delays in approval. The controversy continues still with sales of
Provenge much lower than projections leading to staffing reductions and changes
in management.
The
IMPACT trial that served as the basis for licensing approval of Sipuleucel-T by
the FDA enrolled patients with metastatic androgen independent prostate cancer
(AIPC) also known as hormone resistant prostate cancer (HRPC) It was claimed that
the median survival time for Sipuleucel-T patients was 25.8 months comparing to
21.7 months for placebo-treated patients- a statistical significant period of
four months.
Some doubts have been cast regarding the data presented by
Dendreon. Two articles in this connection are NEW
DOUBTS ABOUT PROSTATE-CANCER VACCINE PROVENGE (March 2012) and
THE
PROVENGE VACCINE & A DISCREPANCY OVER DATA (November 2012).
 Positive
consequences of Provenge: Positive
consequences of Provenge:
- Dendreon point to four months increase in survival in men treated with
Sipuleucel-T over men in the IMPACT study. The survival times of 25.8 and 21.7
months respectively are the median survival periods. In other words half the men
in each arm of the study died within the median periods while the other half did
not die within that period.
 Negative consequences
of Provenge:
Negative consequences
of Provenge:
- Most negative consequences reported were limited to chills, fever, fatigue,
nausea and headache occurring within the first few days of each round of treatment.
- Men
in the Sipuleucel-T arm of the IMPACT study had 50% more serious cardiovascular
events than those in the placebo arm.
BACK
TO INDEX
| RADIATION
- BRACHYTHERAPY SEED
IMPLANTS and HIGH DOSAGE RADIATION | Radiation
therapy is most commonly by way of EXTERNAL BEAM
RADIATION THERAPY (EBRT). This means that the radiation is generated
outside the body and focused on the tumor. One of the concerns about EBRT (external
beam radiation therapy) is that there is a potential for damage to other parts
of the body through which the beam must pass. Brachytherapy on the other hand
involves the insertion of radioactive seeds into the gland adjacent to the tumor
with the aim of limiting consequential damage to other organs. There are some
concerns in brachytherapy relating to the precise placement of the radioactive
seeds and the potential movement of the seeds. Some practitioners use what is
termed 'stranding' where the seeds to be implanted are placed in a degradable
sheath. Others implant seeds individually. The seeds are each about the size of
a grain of rice. They are either left in the gland permanently (this is commonly
known as SI - seed implants) or seeds with a higher radiation dosage are inserted
for a limited time and then removed (this is known as HDR - high dosage radiation). Brachytherapy
is usually considered as an alternative to surgery for men with a suitable diagnosis
- usually men with a PSA below 10 with no palpable disease, and who have a Gleason
Grade no greater than 6 or 7a. Brachytherapy is not a good option for a man who
has previously had a TURP (Transurethral Resection of the Prostate), who has a
very large or very small prostate gland or who has a history of urinary tract
infections (UTI). 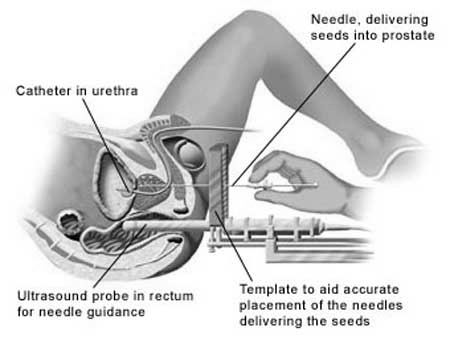 Both
SI and HDR procedures approach the gland through the perineum - the area between
the anus and the genitals. An array of 15-20 thin plastic needles are used to
deliver the seeds into the designated position. In the SI procedure the seeds
are left in place; in the HDR procedure the seeds are withdrawn after a few minutes,
having delivered the measured dose. SI is a relatively short procedure, taking
two or three hours; HDR usually requires four treatments, lasting a few minutes
each, given over two days. The man can go home and carry on with his normal activities
immediately after SI; HDR might need an overnight stay in hospital. There is sometimes
a feeling of fatigue, as is the case with EBRT, but this usually recedes with
time, as the dosage from the seeds reduces (they are only fully active for about
six months).
Both
SI and HDR procedures approach the gland through the perineum - the area between
the anus and the genitals. An array of 15-20 thin plastic needles are used to
deliver the seeds into the designated position. In the SI procedure the seeds
are left in place; in the HDR procedure the seeds are withdrawn after a few minutes,
having delivered the measured dose. SI is a relatively short procedure, taking
two or three hours; HDR usually requires four treatments, lasting a few minutes
each, given over two days. The man can go home and carry on with his normal activities
immediately after SI; HDR might need an overnight stay in hospital. There is sometimes
a feeling of fatigue, as is the case with EBRT, but this usually recedes with
time, as the dosage from the seeds reduces (they are only fully active for about
six months).
There
are many variations to the basic procedures. As mentioned in ANDROGEN
DEPRIVATION THERAPY (ADT), medication might be prescribed before
brachytherapy (often to reduce the size of the gland and possibly make the cancer
cells more susceptible to radiation damage). This is known as neo-adjuvant therapy.
The medication may also be taken after the procedure, the intention being to weaken
any tumor cells or to deal with any cells outside the range of the radiation.
Another major variance in the standard brachytherapy procedures is to combine
brachytherapy with EXTERNAL
BEAM RADIATION THERAPY (EBRT).  Positive
consequences of brachytherapy:
Positive
consequences of brachytherapy:
- Success or "cure" for radiation treatments is measured by a gradual reduction
in PSA level in the months after treatment is completed. The aim is to achieve
a nadir, or low point, of 0.200 ng/ml and to maintain that level. Some authorities
feel a nadir of under 1.00 ng/ml is an acceptable level. Some men experience what
is referred to as a "bump" about 18 months after radiation when the PSA rises
and then falls again. The time taken to achieve a nadir varies considerably.
- No
formal studies have demonstrated the superiority of radiation therapy over other
forms of therapy, including Active Surveillance in appropriate cases. There is
a failure rate of about 30% - 35% over a period of 10 - 15 years for men undergoing
radiation therapy. This may appear to be a higher overall rate than for some other
therapies. That is likely to be because generally men choosing radiation therapies
are older and may have more advanced disease than those choosing other therapies.
- Cryotherapy
can be used as a salvage therapy in the event of failure of initial therapy.
 Negative
consequences of brachytherapy: Negative
consequences of brachytherapy:
Short
Term:
- The entry of needles in the perineum can cause irritation, swelling
and inflammation in this and the genital areas. This usually responds to icing
and anti-inflammatory drugs.
- Fluid can also collect in the scrotum, although
this is more rare. Medical help should be sought.
- There may be some itching
and burning during urination in the immediate aftermath of the treatment as well
as some urgency and blood in the urine. These consequences usually dissipate over
a few days. If they do not medical help should be sought.
- Ejaculate is
likely to be affected in volume, texture and appearance. This may revert to a
normal ejaculate over time.
- In the case of SI procedures, seeds may become
dislodged before healing is complete and move into the urethra. Cases have been
reported of seeds migrating to the bloodstream and lodging in the lungs. This
occurrence appears to be rare and it is claimed that it does not involve any danger.
The prospect of seeds migrating is negated if the stranding procedure is used.
If the seeds are not stranded, it is suggested that a condom be worn after the
procedure and urination should be through a mesh sieve until healing is complete.
- There
is some concern in some quarters about the potential of radiation from implanted
seeds causing damage to people in close proximity to the man after the procedure.
Some practitioners insist on the wearing of lead underpants for the half life
of the seeds; others suggest that young children should not sit on the lap of
the man during this period; others claim that any residual radiation is less than
that experience in an aircraft.
Long
Term:
- The incidence of Erectile Dysfunction (ED) - the inability to have an
erection - is reportedly similar to other therapies. This ED may occur over a
period of time, in contrast to surgery where the immediate loss of erectile function
may be regained over a period of time.
- It is highly probable that even
if the ejaculate reverts to normality, it will not contain active spermatozoa.
Anyone considering radiation therapy who may wish to father a child should consider
using a sperm bank prior to the start of the procedure.
- In the event of
recurrence or failure of radiation treatment, surgery is not a good option and
is rarely successful because of the damage done to the tissue by the procedure.
The usual option for further management is ANDROGEN
DEPRIVATION THERAPY (ADT). Although it is claimed that CRYOTHERAPY
can also be used as a salvage treatment, this might create complications
after brachytherapy. .
- Most urinary problems that might arise are likely
to be short term as listed above, but long term complications of urinary urgency/frequency,
difficulty in starting a urine stream and incontinence may arise over time as
the radioactivity continues to destroy cells.
- Radiation therapies can
sometimes result in bowel incontinence - the inability to control the bowel -
as well as rectal bleeding. The reported incidence of bowel incontinence is fairly
low for brachytherapy, but some bleeding may start in the longer term.
There
is a very thorough explanation of the procedure and outcomes in a specific study
at BRACHYTHERAPY
IN LOCALIZED PROSTATE CANCER. This study is comparatively long
term, since it was commenced in 1998 and the median period reviewed is 7.5 years,
which is to say that half the men in the study were treated more than seven and
a half years ago. A word of warning for this, and any study you might read, the
devil is in the detail and the definitions. When it is claimed that the "...percentage
is 65% average on preserving sexual function over these 7.5 years." and
therefore better than other practitioners, you would need to know precise definitions
of what 'sexual function' means in this study.
For more specific information you may care to visit the SEEDPODS
WEBSITE and for an interesting insight into how a decision to opt
for brachytherapy was made as long ago as 1996 you can read how Andy
Grove went about his research in his article
TAKING
ON PROSTATE CANCER. BACK
TO INDEX
| RADIATION
- EXTERNAL BEAM INCLUDES:
CALYPSO®: CYBERKNIFE®: DART®: PROSTRCISION®: PROTON BEAM: SBRT |
External
beam radiation is known by many acronyms - EBR or EBRT being the most common.
In this treatment a stream of photons or protons is aimed at the prostate gland.
The intention is to damage the DNA of the cancerous cells, leading to their death
over time. There is inevitably some risk of damage to the healthy cells in the
prostate and the surrounding tissue. To minimize the negative consequences of
this collateral damage, the total radiation dose (which is measured in Greys,
expressed as Gy) is fractionated i.e. divided into smaller doses. This means that
the treatment is spread over a relatively long period, normally once a day, five
days a week for seven weeks. However there are many variances to this 'standard',
including HYPOFRACTIONATED THERAPIES,
where a much greater fraction of a smaller total dose is used at each session.
There is a greater risk of collateral damage with these therapies unless the beam
is aimed extremely accurately, but since there are fewer sessions, there is a
benefit of convenience for the man undergoing the therapy - and increased turnover for the supplier of the service.
CyberKnife is a brand name for a device that delivers stereotactic body radiation therapy (SBRT).
There
are many variables that can be very confusing for the newly diagnosed man. This
section is subdivided into three sections:  AIMING BEAMS AND DELIVERY OF DOSES - including
references to Calypso®: Cyberknife®: DART®
AIMING BEAMS AND DELIVERY OF DOSES - including
references to Calypso®: Cyberknife®: DART®
 PROTON BEAM V PHOTON BEAM
PROTON BEAM V PHOTON BEAM
 ADJUVANT THERAPIES - ADT (Androgen
Deprivation Therapy); Brachytherapy including reference to ProstRcision® and
DART®
ADJUVANT THERAPIES - ADT (Androgen
Deprivation Therapy); Brachytherapy including reference to ProstRcision® and
DART®
 SALVAGE THERAPIES
SALVAGE THERAPIES
- AIMING
BEAMS AND DELIVERY OF DOSES
All
EBRT require the man to undergo what is termed a planning session. This is intended
to plot as accurately as possible the site of the man's prostate and tumors using
CAT or MRI scans. When the older techniques are used, target markers are made
on the man's body. These are usually small tattoos. Yana Mentor MARKKU
LEITSO wrote an amusing piece about this procedure at MARKKU'S
GREAT BIG TATTOO ADVENTURE. The tattoos created aiming points for
the radiation beams. As
time went by there was a recognition that, given the movement of the patient and
the gland, a better delivery system was required. This new system was termed 3D
conformal beam radiation therapy (known as 3DEBRT, 3DCRT ,3DRT, 3DXBRT and no
doubt by other acronyms). Casts were made of the man's body to hold him in the
same position for each session. As the radiation heads in the machines became
more mobile and accurate - the so called stereotactic heads - proposed trajectories
and precise strengths of the multiple beams used in each session were plotted.
The term 'conformal' came from this aim to conform to the plotted beams with the
man in precisely the same position for every one of the 35 or so sessions. Because
there was an increase in accuracy, it was possible to increase the doses delivered
without damaging other parts of the body. Although
the conformal radiation process was a substantial improvement, the beams were
still being aimed at the position where the prostate gland had been when the planning
session was carried out. It could not take into account the day to day movements
of the gland. There are significant movements of the gland caused by the contents
of the bladder or bowel for example, or even by breathing which can move the gland
as much as 3 cm. This led to the next step in improving aim - what was termed
broadly as dynamic adaptive radiation therapy. This INTRODUCTION
gives some background on the development of this process. Initially,
as MRI and CAT scans became more efficient, so called fiducials were introduced
into the prostate gland in much the same way as seeds were implanted in the brachytherapy
procedure. This was through the perineum, the area between the anus and the scrotum.
These fiducials were small metal seeds - usually gold because it is inert - which
showed up very clearly on scans. They were then used as aiming points, initially
before the start of each session and later in real time when the scanners were
linked to the radiation equipment. This
new procedure was termed generally as IMRT (Intensity Modulated Radiation Therapy)
or IGRT (Image Guided Radiation Therapy). A number of institutions created trademarks
to describe their versions of therapies using what were termed dynamic adaptive
radiation therapy. Two of the better known ones are CyberKnife® and DART®. The
next step was the development of the Calypso® 4D process. This takes the fiducials
aiming points one step further by the implant of what might be termed GPS devices.
Very small electronic seeds that signal their position and thus do away with the
necessity of scanning equipment being used. Oregon Health Sciences University
followed RICK DANCER
through his treatment to show men what Calypso Radiation is all about. Rick feels
that if you are looking at this form of treatment, this VIDEO
SERIES may help you. These
advances make it even more difficult to compare the outcome of old EBRT procedures
with modern ones. All that can be said in broad terms is that the newer procedures
are a very significant improvement over the older ones. The most important question
a man considering EBRT can ask is how the beams will be aimed and monitored to
ensure an accurate delivery, especially if a hypofractionated dosage is planned.
- PROTON BEAM V PHOTON BEAM
Although
there is only one letter difference between proton beam therapy and photon beam
therapy, advocates of the latter believe that there is a substantial difference
in the consequences. Most
men do not have the relevant ability to fully understand and evaluate the difference
between the therapies based on these options. At a very basic level it can be
said that photons (more commonly known as X-rays) are electromagnetic waves that
have no mass or charge. Protons are large, positively charged particles. Where
the critical difference lies is that photon beams aimed at a tumor in the prostate
gland not only penetrate and act on the tissue they pass through on the way to
the target, they then continue through the target and the tissue beyond that.
To minimize damage to tissue on each side of the prostate gland the proton beams
are fractionated and beamed from a variety of angles through the stereotactic
heads. These beams cross in the gland. That means that the gland gets the full
dose aimed at it, while other tissues gets smaller doses which do less damage. Proton
beams on the other hand can be controlled as to the depth of penetration. They
deposit a large share of their dose in the “Bragg peak” over a relatively short
distance close to the end of the particle’s track in tissue. Beyond the Bragg
peak, which is managed by the relative energy of the beam, protons deliver almost
no additional exit dose. The ability to 'stop' the beam at the prostate gland
means that tissue beyond the gland is spared large doses of radiation. This would
allow proton beams to effectively spare critical structures that are located very
close to the target. This is a simplistic lay person's understanding of these
processes. There is far more complex information available on the Internet. Some
links are provided below.
THE NATIONAL
ASSOCIATION FOR PROTON THERAPY has further information and you
can find the clinics offering proton beam therapy in the United States of America
on the site. Men who are not insured or whose insurers will still not pay for
PBT will discover that it can be a very expensive option. Men who wish to have
proton beam therapy but are uninsured might consider the NATIONAL
CANCER CENTRE IN SEOUL, KOREA An eight-week course of proton treatment
there costs $54,000, still a large sum for most people but less than the US centers.
There is a Proton Beam facility in South Africa - iTHEMBA
but it seems that this is not yet used for prostate cancer. A facility is being
constructed in Australia and it is said it will be ready early in 2014 - details
are at PROTON THERAPY
AUSTRALIA. This site also gives news about proton beam sites around
the world. There
is a significant issue in the background of proton beam therapy which may be worth
understanding. The procedure was been used for many years on a variety of tumors
- notably brain tumors but historically, there was only one institution that used
the procedure for prostate cancer. That was LOMA
LINDA UNIVERSITY MEDICAL CENTER (LLUMC) in California. The procedure
was regarded as 'experimental' by many insurers who declined to pay the cost of
the therapy, which was said to be very much higher than standard photon beam therapy.
Undertaking the treatment regimen at Loam Linda meant that men had to take up
residence for the seven weeks of the treatment. Arrangements were available for
suitable accommodation and for sporting and other activities aimed at helping
the men through the process of dealing with a potentially fatal disease. This
resulted in men developing a collegiate attitude to their time at LOMA Linda,
with many speaking highly of the experience. One of the consequences of this attitude
is that it seems that any criticism or negativity about the therapy may be dampened.
Men who have had the treatment have formed what they call the BROTHERHOOD
OF THE BALLOON. Over 2,000 former proton patients participate on
the site. One of these men - FULLER
JONES - has A STATUS SUMMARY
- MARCH 2008. There is also a highly recommended book written by
Robert J. Marckini entitled YOU
CAN BEAT PROSTATE CANCER AND YOU DON'T NEED SURGERY TO DO IT.
Claims
have been made that the success rate with proton beam therapy is better than photon
beam and that the negative consequences are lower. It is difficult to find long
term data, independently reviewed that demonstrates these claims. Proponents of
proton beam therapy for prostate cancer point to the number of generators that
have been built at a very high cost over the last decade. They say this demonstrates
the efficacy of the therapy. Opponents of proton beam therapy are of the view
that the higher income from this procedure is the driving force behind the wider
availability of the therapy. This is a commentary which followed the release of
data fifteen years after Loma Linda started using proton beam for prostate cancer:
FIRST
DIRECTLY COMPARATIVE DATA QUESTION SAFETY OF PBRT VS. IMRT
Adjuvant
therapies are those that are used in conjunction with the main therapy in the
belief that they will make the main therapy more effective. Such additional therapies
are termed neo-adjuvant if they are used prior to the main therapy commencing. The
most common adjuvant therapy used in conjunction with EBRT is ADT
(ANDROGEN DEPRIVATION THERAPY) This is sometimes used as a neo-adjuvant
therapy (therapy used before the main treatment) to reduce the size of the gland
or because there is a belief that the changes to the cancer cells in the gland
as a result of the ADT will make them more susceptible to damage by the radiation
beams. ADT given after radiation is intended to take care of any cancer cells
that were not in the direct path of the radiation beams but were still in the
immediate vicinity of the gland. The
other major adjuvant therapy is the combining of EBRT and brachtherapy. Although
this double dose approach is carried out in many institutions, two well known
ones are those which have registered trademarks - PROSTRCISION®
and DART®.
It is important to be aware that the claims made on these sites may not be supported
by good independent studies. Advertising claims in the USA are not as subject
to strict rules as in other countries. Anyone considering choosing therapies such
as these should look for other views. For example Dr Chodak has a warning about
ProstRcision in this video BEWARE
OF MISLEADING INFORMATION while an interesting commentary WONDEROUS
SURVIVAL DATA IN LOW-RISK MEN TREATED WITH PROSTRCISION was published
in October 2012 after data was finally released about this therapy. Dattoli
Cancer Center registered their version of the combined EBRT/brachytherapy process
as an acronym of the term Dynamic Adaptive Radiation Therapy,
although this term applies to many other variations of radiotherapy as discussed
above. There are no such commentaries at this time on DART® because there
have been no substantive independent studies to test the claims on the Dattoli
Cancer Center site. One study referred to on the site is in respect of men treated
between 1992 and 1997. This was before DART® was developed. There have been
many changes in the delivery of radiotherapy since then. A Google search shows
that almost every reference to DART® is on the Dattoli website or generated
by them. As
is the case with every aspect of prostate cancer, there is no agreement on the
precise value of adjuvant therapies.The
AUA (American Urological Association) and ASTRO (American Society of Radiation
Oncology) released revised guidelines regarding the application of adjuvant radiation
therapy in May 2013. You can read them here ADJUVANT
AND SALVAGE RADIOTHERAPY AFTER PROSTATECTOMY: ASTRO/AUA GUIDELINE.
- SALVAGE RADIATION THERAPY (SRT)
Many
men, in making their treatment choice (especially when choosing surgery) take
into account the view that, in the event of their primary therapy failing, EBRT
is available as an optional so-called 'salvage therapy. The concept behind this
is that, if the disease has escaped from the prostate gland, it may not have ventured
past the organs in the immediate vicinity of the gland and therefore radiating
this area may provide the further probability of 'cure' or long term regression. The
decision to choose radiation after apparently failed surgery is not an easy one,
if only because there is no clear definition of how to define failure. This paper
NINE DECISIONS BEFORE ELECTING
RADIATION THERAPY AFTER RADICAL PROSTATECTOMY may be helpful in
making this difficult decision. It also contains information that might be of
interest to anyone consideration EBRT. The AUA (American Urological Association)
and ASTRO (American Society of Radiation Oncology) released revised guidelines
regarding the application of SRT (Salvage Radiation Therapy) in May 2013. You
can read them here ADJUVANT
AND SALVAGE RADIOTHERAPY AFTER PROSTATECTOMY: ASTRO/AUA GUIDELINE. The
consequences of radiation therapy are usually not seen immediately. They tend
to develop over time. In typical cases it may be two to three years before all
the consequences are fully developed.  Positive consequences of external beam radiation:
Positive consequences of external beam radiation:
- Success or "cure" for radiation treatments is measured by a gradual
reduction in PSA level in the months after treatment is completed. The aim is
to achieve a nadir, or low point, of 0.200 ng/ml and to maintain that level. Some
authorities feel a nadir of under 1.00 ng/ml is an acceptable level. Some men
experience what is referred to as a "bump" about 18 months after radiation when
the PSA rises and then falls again. The time taken to achieve a nadir varies considerably.
- No
formal studies have demonstrated the superiority of radiation therapy over other
forms of therapy, including Active Surveillance in appropriate cases. There is
a failure rate of about 30% - 35% over a period of 10 - 15 years for men undergoing
radiation therapy. This may appear to be a higher overall rate than for some other
therapies. That is likely to be because, generally, men choosing radiation therapies
are older and may have more advanced disease than those choosing other therapies.
 Negative consequences of external beam radiation:
Negative consequences of external beam radiation:
Short
Term:
- Because EBRT procedures (other than hypofractionated procedures) take
place on a daily basis over many weeks there is some disruption to familiar routines.
If proton beam is chosen, it may be necessary to relocated for the time of the
therapy because the number of providers is limited.
- The most common short
term consequence of EBRT is a feeling of fatigue which often grows as the therapy
progresses. Most men do no seem to be badly affected and a nap usually overcomes
the feeling. The fatigue will usually disappear after completion of the therapy.
- Existing
bladder problems may be worsened and urinary retention may be an issue as the
gland swells. In few, but severe cases, catheterisation may be required. It is
for this reason that men with existing problems are counseled against radiation
as an option.
- There may be some bleeding in the rectal area although this
is unusual with modern procedures.
Long
Term:
- The incidence of Erectile Dysfunction (ED) - the inability to have an
erection - is reportedly similar to other therapies. This ED usually occurs over
a period of time, in contrast to surgery where the immediate loss of erectile
function may be regained over a period of time. Because historically men who opted
for radiation therapy tended to be older or more sickly than men who chose surgery,
some of the reported ED may be due to the aging process.
- Ejaculate is
likely to be affected in volume, texture and appearance. It is highly probable
that even if the ejaculate reverts to normality, it will not contain active spermatozoa.
Anyone considering radiation therapy who may wish to father a child should consider
using a sperm bank prior to the start of the procedure.
- In the event of
recurrence or failure of radiation treatment, surgery is not a good option and
is rarely successful because of the damage done to the tissue by the radiation.
The usual option for further management is ANDROGEN
DEPRIVATION THERAPY (ADT). It is claimed that CRYOTHERAPY
can also be used as a salvage treatment.
- Most urinary problems
that might arise are likely to be short term as mentioned above, but long term
complications of urinary urgency/frequency, difficulty in starting a urine stream
and incontinence may arise over time.
- Radiation therapies can sometimes
result in bowel incontinence - the inability to control the bowel - as well as
rectal bleeding. The reported incidence of bowel incontinence is fairly low where
modern equipment is used, but some bleeding may start in the longer term.
- There
is some evidence that EBRT may be associated with the development of other cancers,
notably bladder cancer. The studies to date show a very small risk of this consequence.
BACK
TO INDEX
Dr
Gerry Potter is credited with the discovery of Abiraterone Acetate which has been
approved a a therapy for prostate cancer and is now marketed under the trade name
of ZYTIGA. He now claims that
he has discovered another compound which he has named Salvestrols. A
paper titled NUTRITION
AND CANCER: SALVESTROL CASE STUDIES has four authors, including
Dr Potter. The Introduction says how Salvestrols work and says in part
"Salvestrols are a class of phytonutrients that, in humans, are metabolised by
the tumourspecific CYP1B1 enzyme in cancer cells to initiate a cascade of processes,
including apoptosis, that result in the arrest or decline of the cancer…………. We
use them in helping to rid our body of cells that have become cancerous." The
claims made are then supported by reference to what are termed 'Cases'. Case #3
is Prostate Cancer and states: A
seventy-four-year-old gentleman received a PSA test result indicating a level
of 11 ng/ml in the blood following his annual check-up. His previous PSA result
had been 4 ng/ml. The consulting surgeon suspected cancer and advised that surgery
or radiation would be required. A follow-up magnetic resonance scan and full body
X-ray confirmed a diagnosis of prostate cancer. Surgery or radiation were both
ruled out and the patient was prescribed a course of the synthetic hormone leuprorelin
acetate (Prostap®) on a quarterly basis. The patient was advised that this treatment
would be required for the rest of his life.
Subsequently this gentleman
spoke with his cousin, a university lecturer, who told him that one of his students
was diagnosed with a terminal cancer of the brain and after taking Salvestrols
had proved to her doctors that 'terminal' seemed to be an overstatement. He decided
to begin a course of Salvestrol supplementation taking two (350 point) Salvestrol
Professional capsules per day.
Six months after receiving his diagnosis
his PSA level had dropped to below 1 ng/ml. However, during this time the patient
suffered from breast development, complete loss of body hair, impotence and a
complete lack of libido as a result of the synthetic hormones. The patient moving
to another country necessitated a change of doctors. At this point the patient
switched Salvestrol products and began taking one (1,000 point) Salvestrol Professional
capsule per day and one (350 point) Salvestrol Professional capsule three times
per day. Twelve months after receiving his diagnosis his PSA level had dropped
to 0.2 ng/ml.
The new doctor continued with the PSA monitoring and quarterly
injections of Lupron (a different brand of leuprorelin acetate). Upon receiving
a subsequent PSA test result for this patient the attending physician said that
the PSA level received was as low as it could be and asked if the patient was
sure that he had not had surgery! Given the physician's surprise that such a result
could be attributed to leuprorelin acetate alone the patient confessed to taking
Salvestrols. The physician then stated that he had a patient that he would like
to start on Salvestrols and asked the patient to supply him with background information.
The physician decided to 'wean' the patient off of the quarterly Lupron injections.
This patient has not had a Lupron injection for six months and continues
to receive PSA test results at the 0.2 ng/ml level. The patient continues to take
one (350 point) Salvestrol Professional capsule per day and has embarked on a
fitness program and change in diet. There
is a deal of misleading information here: - At least 65% of men with a
PSA of 11 ng/ml will not have a positive biopsy. The most common causes of PSA
readings at this level are BPH (Benign Prostatic Hyperplasia) and prostate/bladder
infections
- It is not possible to diagnosed prostate cancer without a biopsy
procedure: a follow-up magnetic resonance scan and full body X-ray cannot confirm
a diagnosis of prostate cancer.
- It is difficult to establish a time range
for this study, but it would not be unusual for a PSA of 11 ng/ml to revert to
a 'normal' very low level if it was due to BPH (Benign Prostatic Hyperplasia)
following ADT (Androgen Deprivation Therapy) for what appears to be at least eighteen
months
For these reasons it seems appropriate not to accept that this constitutes a 'proof'
that Salvestrols have 'cured' this man.
For more on the subject, go to
TRADEMARKED
SCIENCE TRADE-OFFS. If you do that, please read the comments, which
present some other relevant information.
 Positive
consequences of active salvestrols: Positive
consequences of active salvestrols:
- Salvestrols may well improve overall health. This may then enhance the
immune system to such an extent that the cancer is sent into regression.
- The
consequences of conventional therapies may be lessened or managed better by using
Salvestrols.
 Negative
consequences of active salvestrols:
Negative
consequences of active salvestrols:
- The use of Salvestrols may clash with conventional medication. For this reason,
the use of Salvestrols should always be discussed with medical advisors before
commencing the therapy.
- There is no clear evidence for the efficacy
of Salvestrols in managing prostate cancer.
- Relying on Salvestrols can
result in the disease advancing to a stage where any prospect of cure by conventional
means is lost.
BACK
TO INDEX
|
SURGERY OPEN
MANUAL RADICAL: RETROPUBIC PROSTATECTOMY: PERINEAL PROSTATECTOMY LAPAROSCOPIC
: MANUAL: ROBOTIC ASSISTED (RALP) - DA VINCI | Most
men diagnosed with prostate cancer choose surgery. This is especially true in
the US where surgery is often referred to as the 'gold standard' of all the optional
therapies and choices. It is the treatment most commonly prescribed for younger
men or early stage prostate cancer. The traditional surgery was an 'open' procedure
but there is enormous and rapid growth in laparoscopic - 'keyhole' - surgery,
especially the Da Vinci robotic assisted procedure. There is some disagreement
as to whether it is always in the best interests of men with what is termed LOW
RISK prostate cancer to have surgery before spending time trying
to establish if the disease is one of the indolent types or the more aggressive
types. Prostate
cancer surgery - radical prostatectomy (RP) - is a complex operation and there
are four main optional procedures: two open procedures and two laparoscopic. This
technical document ANATOMICAL
APPROACH TO RADICAL PROSTATECTOMY gives some idea of the major
steps in the procedure. Mayo Clinic announced a new procedure termed NATURAL
ORIFICE TRANSLUMINAL ENDOSCOPIC SURGERY (NOTES)
and removes the prostate gland through the penis in July 2010. It is
difficult to see the advantage of this, which seems to make a complex procedure
even more complex. Apparently there are alternative, but similar procedures, one
of which uses some form of microwave and another that removes the gland through
a small incision in the belly to give access to the bladder. These would all be
regarded as experimental. 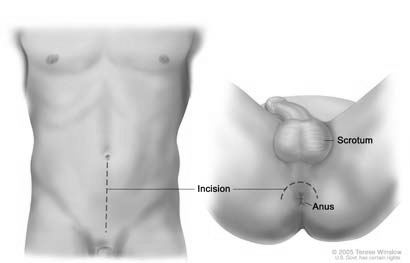  In open surgery, the prostate gland is reached either from the lower part
of the front of the body - this is a retropubic procedure - or through the area
between the anus and the scrotum - this is a perineal procedure. The illustration
shows where the incisions are made in these two procedures. Historically, the
perineal approach was less common than the retropubic. There are no studies that
show either of these procedures to be superior to the other but several claims
were made for each. One of the key claims for retropubic was that it made for
easier access to lymph nodes to check for progression. It is now very unusual
to carry out this check. The supporters of the perineal approach claimed that
there was less chance of blood loss with this option. Historically the retropubic
operation did indeed involve a substantial loss of blood. Some surgeons recommend
the drawing and storing of the patient's own blood ahead of the operation as a
precautionary measure. However, the significant improvements in surgical techniques
have made it unusual now for a transfusion to be required.
In open surgery, the prostate gland is reached either from the lower part
of the front of the body - this is a retropubic procedure - or through the area
between the anus and the scrotum - this is a perineal procedure. The illustration
shows where the incisions are made in these two procedures. Historically, the
perineal approach was less common than the retropubic. There are no studies that
show either of these procedures to be superior to the other but several claims
were made for each. One of the key claims for retropubic was that it made for
easier access to lymph nodes to check for progression. It is now very unusual
to carry out this check. The supporters of the perineal approach claimed that
there was less chance of blood loss with this option. Historically the retropubic
operation did indeed involve a substantial loss of blood. Some surgeons recommend
the drawing and storing of the patient's own blood ahead of the operation as a
precautionary measure. However, the significant improvements in surgical techniques
have made it unusual now for a transfusion to be required.
  Laparoscopic surgery on the other hand requires five small ( five to 10
millimeters) incisions (or portholes), one just above or below the belly button
and two each on both sides of the lower abdomen. Four arms are inserted into the
portholes, three hold instruments, the fourth holds the camera - this is the laparoscope
which enables the surgeon to get pictures of the prostate on a video monitor.
Manual laparoscopic procedures have been described like operating with knitting
needles. The arms used are straight rods which make it difficult in some cases
to reach the entire gland, given the variability in size and precise placement
of the gland in the body. The arms used in the robotic assisted procedure are
flexible and this restriction of reach would only apply in unusual cases.
Laparoscopic surgery on the other hand requires five small ( five to 10
millimeters) incisions (or portholes), one just above or below the belly button
and two each on both sides of the lower abdomen. Four arms are inserted into the
portholes, three hold instruments, the fourth holds the camera - this is the laparoscope
which enables the surgeon to get pictures of the prostate on a video monitor.
Manual laparoscopic procedures have been described like operating with knitting
needles. The arms used are straight rods which make it difficult in some cases
to reach the entire gland, given the variability in size and precise placement
of the gland in the body. The arms used in the robotic assisted procedure are
flexible and this restriction of reach would only apply in unusual cases.
 In
laparoscopic
prostatectomy, the man is positioned in the so-called Trendelenburg position,
with spread legs and feet higher than the head. This slight slant shifts the organs
located in the abdomen towards the head, which provides the surgeon with more
room in the pelvic area. Carbon dioxide is passed into the abdominal cavity through
a small tube placed into the incision below the belly button. This gas lifts the
abdominal wall to give the surgeon a better view of the abdominal cavity once
the laparoscope is in place. The operating arms are used by the surgeon to remove
the gland, through one of the portholes. When the procedure is robotic assisted
- the so-called Da Vinci procedure - the surgeon sits at a console away from the
operating table. He views the procedure by looking at the 3-D images from the
laparoscope. The operating arms are maneuvered with two foot pedals and two hand
controllers, translating the the surgeon's movements into precise micro-movements
of the instruments. In
laparoscopic
prostatectomy, the man is positioned in the so-called Trendelenburg position,
with spread legs and feet higher than the head. This slight slant shifts the organs
located in the abdomen towards the head, which provides the surgeon with more
room in the pelvic area. Carbon dioxide is passed into the abdominal cavity through
a small tube placed into the incision below the belly button. This gas lifts the
abdominal wall to give the surgeon a better view of the abdominal cavity once
the laparoscope is in place. The operating arms are used by the surgeon to remove
the gland, through one of the portholes. When the procedure is robotic assisted
- the so-called Da Vinci procedure - the surgeon sits at a console away from the
operating table. He views the procedure by looking at the 3-D images from the
laparoscope. The operating arms are maneuvered with two foot pedals and two hand
controllers, translating the the surgeon's movements into precise micro-movements
of the instruments.
RP
(radical prostatectomy), whether open or laparoscopic, is a major surgical procedure
and will usually take 3 - 4 hours. Discharge from hospital was historically within
3 to 5 days for the 'open' procedures but is now likely to be 2 or less. Laparoscopic
surgery, on the other hand, is far less traumatic and men are usually discharged
from hospital in 24 hours. There is still a good deal of disagreement about the
merits of the two procedures. Surgeons favoring open surgery say that they can
feel the prostate and get a better idea of where the tumor might be and thus have
more assurance of negative margins: doctors favoring laparoscopic surgery say
that the better view obtained through the magnifying lens enables them to cut
and stitch more accurately. As yet there are no long term studies to support either
view. Commentaries on some relevant studies, which are linked from the commentaries,
published since 2010 are listed below. It appears that the incidence of initial
negative consequences with laproscopic procedures are similar to those with open
procedures, as are early biochemical failure rates.  Vattikuti Urology Institute October 2010: 5-YEAR
OUTCOMES OF PATIENTS TREATED WITH RALP
Vattikuti Urology Institute October 2010: 5-YEAR
OUTCOMES OF PATIENTS TREATED WITH RALP
 European Urology March 2011: QUALITY
OF OUTCOMES AFTER FIRST-LINE RP
European Urology March 2011: QUALITY
OF OUTCOMES AFTER FIRST-LINE RP
 Journal for Healthcare Quality July 2011: ARE
CLINICAL BENEFITS OF RALP BEING OVER-HYPED?
Journal for Healthcare Quality July 2011: ARE
CLINICAL BENEFITS OF RALP BEING OVER-HYPED?
 Massachusetts General February 2012 : RALP
NOT ASSOCIATED WITH BETTER CONTINENCE, SEXUAL FUNCTION
Massachusetts General February 2012 : RALP
NOT ASSOCIATED WITH BETTER CONTINENCE, SEXUAL FUNCTION
 European Urology April 2012: SHORT-TERM
OUTCOMES OF RALP COMPARED TO OPEN SURGERY
European Urology April 2012: SHORT-TERM
OUTCOMES OF RALP COMPARED TO OPEN SURGERY
 European Urology October 2012: CONTINENCE
AND SEXUAL FUNCTION AFTER RALP COMPARED TO LRP
European Urology October 2012: CONTINENCE
AND SEXUAL FUNCTION AFTER RALP COMPARED TO LRP
One
thing has become clear - the learning curve for the laparoscopic procedure is
a long one. One published study implies that it takes at least 250 procedures
before the surgeon can be regarded as proficient. Once a decision has been made
to proceed with surgery and which optional surgical procedure is likely to produce
the best result, the next step is the selection of the surgeon to carry it out.
There is evidence that the expertise of the medical team carrying out a procedure
has a direct bearing on the likely outcome. The more experienced the surgeon,
the less the likelihood of negative consequences. Dr Arnon Krongrad is a prostate
cancer surgeon. He has written a piece which may help in finding the right surgeon:
HOW
TO PICK A PROSTATE CANCER SURGEON - the same principles would apply
to choosing any medical team.
Two long term survivors of the disease maintain lists of what they term the best
surgeons and specialists. Contact details are on the RESOURCES
page.  Positive consequences of surgery:
Positive consequences of surgery:
- Surgery can introduce an element of certainty. The entire prostate gland
can be examined closely to establish the extent of the tumor, to verify the Gleason
Score and to clarify the likelihood of the tumor being contained within the gland.
- If
there has been no spread beyond the gland, then the removal of the prostate should,
by definition, remove the tumor For many men that is of utmost importance.
- In
the event of recurrence or failure, it is possible to use EBRT
(EXTERNAL BEAM RADIATION THERAPY) as what is termed a salvage therapy
to treat recurrence thought to be confined to the prostate bed, or to use ADT
(ANDROGEN DEPRIVATION THERAPY) as a secondary treatment for recurrence
where the disease has spread into other areas of the body. There are also claims
that CRYOTHERAPY can be used
for salvage therapy.
 Negative
consequences of surgery:
Negative
consequences of surgery:
Short
term:
- The most significant negative consequence of of surgery is erectile dysfunction
(ED - the difficulty or inability to have an erection). This comes about because
the nerves controlling erections are embedded near the surface of the prostate
gland; one set on each side. Short term ED occurs in almost 100% of men immediately
after surgery, but will improve in many men as time goes by. There is a view that
the use of drugs or injections to stimulate erections as soon as is safe after
surgery may help to improve the long term outcome - see USE
IT OR LOSE IT. Recovery of erectile function will almost certainly
take many months and sometimes a year or more. Recovery of erectile function is
dependent to a large extent on the ability of the surgeon to spare the erectile
nerves, although this is not the only factor.
- Bladder incontinence (the
inability to control the bladder) is the second most significant negative consequence.
A catheter will be in place, usually for some weeks after the surgery. It normally
takes some time - typically about three months, although this can vary considerably
- to regain control of the bladder function.
- There may be some short period
shoulder and neck problems after surgery in the Trendelenburg position, especially
if there is a pre-existing condition which may be exacerbated by having the body
in this position.
- There is often a considerable degree of discomfort with
gas, which is why men are encouraged to start walking as soon as they can do so
in comfort. As is the case with horses, such movement helps in releasing the gas.
There is a view that the carbon dioxide used in some procedures is the cause of
this problem, but the expert view is that the unusual angle of the body for some
hours traps normal gas in the gut.
Long
term:
- The Gleason Score established after examining the entire gland may differ
from the biopsy score. About one third will be found to be higher and about one
third lower. Dr. Peter Scardino, author and specialist at Memorial Sloan-Kettering
was quoted as saying that there was no guarantee that surgery would actually find
cancer. He said in part [MSK] "...... looked at 2,000 patients whose prostates
were removed during the last four years, after biopsies said they had cancer.
But in more than 30% of the cases, the prostate removed either had microscopic
amounts that weren't life-threatening, or no cancer at all.....in some cases,
cells removed in biopsies were cancerous, but the rest of the prostate appeared
cancer-free."
- The finding of no positive margins is taken to
show that the disease has not spread beyond the prostate gland. Success or "cure"
is measured by taking PSA tests at intervals after the surgery. Ideally there
should be no PSA measurement detectable with the normal PSA test. ULTRA-SENSITIVE
PSA tests may show very low levels - well below 0.10 ng/ml.
- No
formal studies have demonstrated the superiority of surgery over other forms of
therapy, including Active Surveillance, in early stage cancer. There is a failure
rate of about 30% - 35% over a period of 10 - 15 years for men undergoing surgery.
Some failures have been reported at 20 years. In the event of recurrence or failure
of the treatment, it is possible to use EBRT (External Beam Radiation Therapy)
to treat recurrence thought to be confined to the prostate bed, or to use ADT
(Androgen Deprivation Therapy) as a secondary treatment for recurrence where the
disease has spread into other areas of the body.
- There are claims of a
reduction in the reported rates of long term ED (erectile dysfunction) following
the development of what is referred to as the "nerve-sparing" technique and the
use of pharmaceutical drugs such as Cialis, Levitra or Viagra or one of the injectable
materials - MUSE, Tri-Mix and the like. However, the position of the tumor may
affect the ability of even the best surgeon to spare one or both of the nerves
while removing all the cancer. The long term ED rate is still high - probably
over 50%, especially for men over the age of 50. Studies quoted with better rates
should be examined very carefully, especially for definitions of potency or erectile
function. One recent study defined satisfactory recovery of erectile function
as "...the ability to achieve and maintain satisfactory erections firm enough
for sexual intercourse in more than 50% of attempts, with or without the use of
drugs like Viagra or Cialis or Levitra." The published studies usually involve
excellent surgeons and may not reflect the general outcome of surgeries carried
out by surgeons with less experience.
- Long term total bladder incontinence
is reported in a small number of men - about 5% - but many men experience some
leakage when lifting, coughing, sneezing or laughing. Again it is important to
look at definitions in studies showing levels of continence after treatment. It
is not uncommon for the use of 'only' one or two pads a day to be regarded as
fully continent in such studies. The outcomes of surgery carried out by urologists
who do not have the experience of surgeons in a centre of excellence are usually
worse than the results shown in published studies.
- CLIMACTURIA
- the leakage of urine at climax for men who are able to achieve
sexual activity after surgery is not discussed very often on prostate cancer sites
and this can lead men to believe that they are one of the few men to have this
problem. One study suggests that 50% of men may have to deal with this issue.
- PENILE
SHRINKAGE is also reported in a significant number of men, thought
to be the result of maintaining the penis in the flaccid state during what can
be many months of recovery of erectile function. It is thought this can be counteracted
by stimulating erections with drugs or manual devices as soon as post-surgical
healing has taken place.
- PEYRONIES
DISEASE or Peyronie's Syndrome occurs in a surprising number of
men who have had surgery. This condition is one where the erect penis acquires
a 'bend' or deflection. The vast majority of Peyronie cases are very mild but
others can cause severe problems. It seems unlikely that the condition is directly
caused by a disease, or that it has any direct link with prostate cancer. A common
cause is thought to arise from accidents during sexual activities, especially
if the penis is not fully erect.
- Stricture from scar tissue can also cause
long term urinary problems. If the man has a history of poor scarring (some reports
suggest that if any scar on his body is more than 10 mm (about 3/8") wide) then
there is about an eightfold increase in urinary problems following RP (Radical
Prostatectomy).
- Since there is no ejaculate following the removal of the
prostate gland men are infertile, although it may be possible to recover spermatozoa
from the testes. Men intending to father children should consider banking sperm
before surgery.
Men
choosing this option might find it helpful to visit these links:
Another
aspect of Surgery that often causes some concern ahead of the procedure is the
likely effect on sexual ability. These are three pieces written by men based on
their personal experiences that might be useful reading:  SEX AFTER RADICAL PROSTATECTOMY
SEX AFTER RADICAL PROSTATECTOMY
 SEX AND PROSTATE CANCER
SEX AND PROSTATE CANCER
 ERECTIONS - WHAT MOST
MEN WON'T TALK ABOUT BUT THEY ALL WANT TO KNOW ABOUT
ERECTIONS - WHAT MOST
MEN WON'T TALK ABOUT BUT THEY ALL WANT TO KNOW ABOUT
Husband
and wife team Stephan Wilkinson and Susan Crandell contributed their views on
erectile dysfunction for a book OVER
THE HILL AND BETWEEN THE SHEETS: SEX, LOVE AND LUST IN MIDDLE AGE
after Stephan's radical prostatectomy. These excellent pieces written
by them show clearly some of the differences between the way men and women regard
the issue and are well worth reading.  Susan's essay is WHAT'S SEX GOT TO DO
WITH IT? and
Susan's essay is WHAT'S SEX GOT TO DO
WITH IT? and
 Stephan's is entitled MECHANICAL
FAILURE.
Stephan's is entitled MECHANICAL
FAILURE.
 Sex therapist Bettina Arndt collected data from a number of men on the site for
her book WHAT MEN WANT - IN BED
is all about why sex matters so much to men
Sex therapist Bettina Arndt collected data from a number of men on the site for
her book WHAT MEN WANT - IN BED
is all about why sex matters so much to men
BACK
TO INDEX
Abiraterone
was approved by the US Food and Drug Administration (FDA) in April 2011. The trial
used to gain approval was for men with late stage metastasized prostate cancer
which was castration-resistant (also know as hormone-resistant or hormone-refractory
prostate cancer) which had not responded to chemotherapy. For commentary on a
trial in men who had not yet used chemotherapy see
ABIRATERONE ACETATE IN CHEMOTHERAPY-NAIVE MCRPC - PHASE III
TRIAL OUTCOME. Abiraterone is marketed under the trade name Zytiga
in combination with prednisone or prednisolone. There are no studies to indicate
what the long term consequences are of taking Zytiga. The short term approval
studies show the following consequences:  Positive consequences of Zytiga:
Positive consequences of Zytiga:
- An extended median survival of 14.8 months against the 11.2 months of
the men on a placebo.
- A decline in prostate specific antigen (PSA) in
up to 70% of patients as well as some shrinkage of tumors and some symptom improvement.
 Negative consequences
of Zytiga: Negative consequences
of Zytiga:
- It is extremely important to follow strict rules in taking Zytiga. No
food should be eaten two hours before and one hour after taking the daily dose.
- Heart
Problems: High blood pressure (hypertension), low blood potassium levels (hypokalemia),
and fluid retention (edema). Men with existing heart problems must present a full
medical history before considering Zytiga.
- Liver problems: Blood tests
to check liver function must be carried out before and during treatment.
- Minor
issues include: Joint swelling or pain; Muscle aches; Hot flushes; Diarrhea; Urinary
tract infection; Cough; Irregular heartbeats; Urinating more often than normal/need
to get up at night to urinate; Heartburn; Cold-like symptoms; Bone fractures.
- Adrenal
problems may occur.
Studies
are being undertaken to evaluate the use of Zytiga by men who do not yet have
metastasized or castration-resistant disease. One small short term study looks
promising.
Last Updated: March 8, 2019
BACK
TO INDEX The
last of the pages in this section of the site is next - RESOURCES.
There you will find links to other sites where you can find more detailed and
varied information. All this should give you a better understanding of your diagnosis
and help you make the decision that is best for you.
|



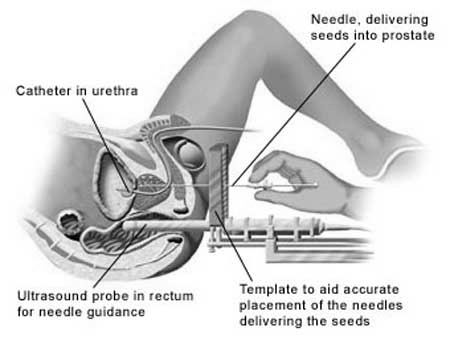 Both
SI and HDR procedures approach the gland through the perineum - the area between
the anus and the genitals. An array of 15-20 thin plastic needles are used to
deliver the seeds into the designated position. In the SI procedure the seeds
are left in place; in the HDR procedure the seeds are withdrawn after a few minutes,
having delivered the measured dose. SI is a relatively short procedure, taking
two or three hours; HDR usually requires four treatments, lasting a few minutes
each, given over two days. The man can go home and carry on with his normal activities
immediately after SI; HDR might need an overnight stay in hospital. There is sometimes
a feeling of fatigue, as is the case with EBRT, but this usually recedes with
time, as the dosage from the seeds reduces (they are only fully active for about
six months).
Both
SI and HDR procedures approach the gland through the perineum - the area between
the anus and the genitals. An array of 15-20 thin plastic needles are used to
deliver the seeds into the designated position. In the SI procedure the seeds
are left in place; in the HDR procedure the seeds are withdrawn after a few minutes,
having delivered the measured dose. SI is a relatively short procedure, taking
two or three hours; HDR usually requires four treatments, lasting a few minutes
each, given over two days. The man can go home and carry on with his normal activities
immediately after SI; HDR might need an overnight stay in hospital. There is sometimes
a feeling of fatigue, as is the case with EBRT, but this usually recedes with
time, as the dosage from the seeds reduces (they are only fully active for about
six months).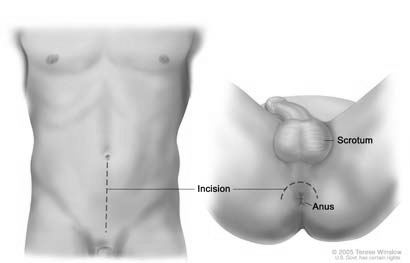

 In
laparoscopic
prostatectomy, the man is positioned in the so-called Trendelenburg position,
with spread legs and feet higher than the head. This slight slant shifts the organs
located in the abdomen towards the head, which provides the surgeon with more
room in the pelvic area. Carbon dioxide is passed into the abdominal cavity through
a small tube placed into the incision below the belly button. This gas lifts the
abdominal wall to give the surgeon a better view of the abdominal cavity once
the laparoscope is in place. The operating arms are used by the surgeon to remove
the gland, through one of the portholes. When the procedure is robotic assisted
- the so-called Da Vinci procedure - the surgeon sits at a console away from the
operating table. He views the procedure by looking at the 3-D images from the
laparoscope. The operating arms are maneuvered with two foot pedals and two hand
controllers, translating the the surgeon's movements into precise micro-movements
of the instruments.
In
laparoscopic
prostatectomy, the man is positioned in the so-called Trendelenburg position,
with spread legs and feet higher than the head. This slight slant shifts the organs
located in the abdomen towards the head, which provides the surgeon with more
room in the pelvic area. Carbon dioxide is passed into the abdominal cavity through
a small tube placed into the incision below the belly button. This gas lifts the
abdominal wall to give the surgeon a better view of the abdominal cavity once
the laparoscope is in place. The operating arms are used by the surgeon to remove
the gland, through one of the portholes. When the procedure is robotic assisted
- the so-called Da Vinci procedure - the surgeon sits at a console away from the
operating table. He views the procedure by looking at the 3-D images from the
laparoscope. The operating arms are maneuvered with two foot pedals and two hand
controllers, translating the the surgeon's movements into precise micro-movements
of the instruments.