Thanks are due to Eric. He came up with the idea of indexing the Survivor Stories that are on the site and did all the preliminary work to set them up.
Being diagnosed with prostate cancer came as one hell of a shock as I had none of the 'typical' symptoms. The first indication I had a 'problem' was in July 2000 when I had my annual medical check-up and my GP ordered the usual blood test. A few days later my GP phoned to say he wanted to see me as one of the blood test results was higher than he'd like. During the consultation he indicated my PSA was 7, and anything over 4 was a concern. He performed a digital rectum examination (DRE) and recommended the name of a Urologist I should see ASAP.
My PSA reading two years earlier was 3. Had I known then what a PSA test would detect, there is no doubt I would have not waited so long for my next 'annual' check-up.
At my first appointment with the Urologist, he also performed a DRE and indicated my prostate was enlarged and that I should have a biopsy. He also outlined the three most common forms of treatment for my age (56), ie surgery, hormonal treatment and radiotherapy.
A couple of weeks later I had the ultrasound immediately followed by the biopsy during which the Urologist took 10 core samples. He later said that most Urologists normally only take 6 samples. But by taking an extra 4 samples cancer is often detected which may not be found in the normal 6 cores.
A week or so later the Urologist advised 6 of the 10 were 'positive' and that the cancer was "very aggressive". (There was no mention of a Gleason Score. It was during a subsequent visit after I had read a bit that I asked for and was advised my Gleason Score was 9.)
The next day I had a whole body bone scan and the day after that a pelvic area CAT scan. Although both results indicated "all clear", the Urologist said the aggressive nature of my cancer worried him and recommended a pelvic lymph node dissection. This involved keyhole surgery under general anaesthetic and an overnight stay in hospital.
There are two forms of a Radical Prostatectomy. One method involves an incision through the abdomen where the surgeon will first remove the pelvic lymph nodes, send them off to the pathologist while the patient is still under anaesthetic, then either continue with or abort the prostatectomy depending on the result. The 'perineal' method (described later) involves the need for a separate operation to remove and check the pelvic lymph nodes but has the advantage that the pathology is not 'rushed'.
Three days later the Urologist advised no cancer cells were detected in lymph nodes, so there was some probability the cancer had not escaped the prostate. He indicated all treatment options were open to me - but the decision was mine to make. He showed me a 'Partin Table' that indicated with Gleason 9 there was only a 30% chance of success ie. he could "get it all" with surgery. He suggested I see an Oncologist with whom he had discussed my case. The Oncologist indicated statistics showed a 70% success rate with 3 months of hormone treatment followed by 7 weeks of radiotherapy then 3 more years of hormone treatment. Despite this promising information some of the side effects worried me a little so I decided to read some more. I also went to a local Support Group meeting. But I found the information I was reading and hearing confusing and sometimes contradictory. But all agreed that I had to believe the treatment I decided on was 'right' for me.
I eventually chose surgery. Why? It appeared to me the best sequence of treatments, then if required, radiotherapy followed by hormone treatment if all else failed. I felt this would give me "three bites of the cherry" - if I needed them and perhaps a better chance of a successful outcome.
On the Monday 16th October 2000, the Urologist started a Radical 'Perineal' Prostatectomy. This involved a 'U' shaped incision between the scrotum and anus and a separate incision for a drain tube. Later that day the Urologist came to see me and said all went well, ie. there was little loss of blood so there was no need for a blood transfusion (I had given two units of blood just in case) and the prostate had come out 'nicely' (what ever that was supposed to mean). The day after surgery all seemed to be going well - there was no sign of infection and none of the pain I was told to expect - just a little 'discomfort' when passing 'wind'. Breakfast was fluids only but I was upgraded to a light diet lunch and dinner.
On the second day (post operation) something happened that I don't recall reading about in any of the books or YANA Journals. I suddenly became very emotional (yes, openly crying). The nurses did their best to calm me down by suggesting it was probably due to a build up of a number of things, ie stress incurred during the treatment decision process, anxiety about surgery, worrying about the forthcoming pathology result or about being emotional. They tried to assure me that getting emotional was just part of the healing process after the trauma of major surgery. When things got the better of me again the following day, they suggested and I agreed to a visit from a social worker. The social worker also told me it was "quite normal" to get emotional (not for me it's not, I was still thinking!!) and what I was going through emotionally was very much like loosing a loved one (wife, child) that is, I was grieving - for the loss of the person I was before being diagnosed with cancer. This seemed to make sense and I guess I started to believe what they were all telling me and not what I was thinking, ie that I was "losing my mind".
Just after lunch on the Friday, four days after the operation, my Urologist arrived with the pathology result. He said there was a lot of cancer in the prostate but the majority was Gleason 7, only a couple of bits were Gleason 9. Also in two areas the cancer was at the edge but there were no surgical margins. He then suggested I should "go home" to continue the recovery process but it was OK to stay longer in hospital if I wanted to - I was home by 3pm. The drain tube had been removed the previous day but I went home with a catheter in place.
Ten days after the operation the staples (clips) were removed from the main incision area and I was advised that all was healing up OK. A watery fluid and occasional blood was still draining from the separate incision but I was told this would stop in a day or two. Five days later the catheter was removed and an X ray was used to check the area where urethra had been rejoined to the bladder. This indicated all was well but now came the time I was most concerned about, ie. being incontinent. My Urologist simply said expect to be 'wet' for a few days or possibly longer.
I am happy to say that incontinence has not been a problem. The 'other' side effect, impotence is currently a problem but does not greatly concern me at this stage. I almost feel like my 'old' self again in body and mind and although the pathology result was much better than I expected I guess I know that I am not "out of the woods" yet. I will wait with bated breath for the next few PSA tests. But for now things are looking up and I know with some certainty where things stand - which was another reason for choosing surgery.
Some have said I have been 'lucky'. Pam and I now believe it was the great support and the prayers of all my family and friends that has got the better-than-expected result (to date) for me and inner calm for Pam through the 'ordeal'.
[Update 18 December 2000] PSA currently "less that 0.1", next blood test in 3 months.
[Update March 2001] Current PSA remains at less than 0.1.
[Update March 2002] Current PSA remains at less than 0.1. Eric is enjoying life to the full.
[Update September 2003] Current PSA remains at less than 0.1.
Eric retired in October 2002 and enjoys spending more time with family, making/editing home and holiday videos, working for his local church, etc, when not tripping around Australia in a caravan. is enjoying life to the full.
[Update December 2004] Eric hasn't had a PSA test lately as he has been too busy travelling around Australia with Pam in their caravan. They had a great time on their 6 month, 27,000 km (16,000 plus miles) journey. They had a great time, took lots of photos and have 25 hrs of as yet unedited video.
[Update March 2005]
My PSA is still less than 0.10 ng/ml - the blood test was ordered along with the usual annual check up stuff by my GP and he gave me the result. I was due to see my Urologist in December 2004 but phoned his receptionist to say my GP had given me my result and would he still want to see me - she said as long as you are OK (no problems you wish to discuss) there's probably no need.
[Update November 2005]
Just confirming I visited my Urologist today and my PSA remains below 0.10 ng/ml. He said it's very rare that PSA has been known to rise after 5 years - post operation but after 10 years it has not occurred to his knowledge. Which is all good news for me and I thank God for his blessing.
[Update November 2006]
Now to the stage were I get a blood test once a year. I phone for the result one year and visit my urologist every other year. Latest result was given to me today by the urologist's nurse who said my PSA was "Normal and you can't get anything better than that!". Haven't had a result quite like that before but it sounds good. :-)
[Update September 2007]
Eric and Pam have become what we Australians call "grey nomads". In a recent mail he says:
We had 6 weeks in New Zealand earlier this year and just returned from 10 weeks around SouthEast Queensland spending much more time in each place - great.
In passing he mentions that his PSA is still undetectable - there is indeed life after PCa!!
[Update December 2008]
Eric and Pam have had another great year for travelling - around Australia in February/March: seven weeks cruising Alaska's Inside Passage on a small ship only 113 passengers and 73 crew - much better than those big ships, then 5 days - Anchorage, Denali N.P and Fairbanks. Then self drive - Vancouver Island, Vancouver, Whistler, Kamloops, Jasper, Lake Louise, Banff, flight to Toronto and then Halifax then back to Vancouver for the 15.5 hr flight home. As a sweetner they had ten days in November on Lord Howe Island. Oh! and as far as his PCa is concerned he says:
All is well with my PSA, ie. still less than 0.1 and cholesterol, sugar, vitamin D and blood pressure are all good but I will continue to have vitamin B12 shots 3 times a year though.
[Update December 2009]
Latest PSA is 0.1 - not less than 0.1 which it has been since 2000 so my GP has suggested an appointment with my Urologist - I'll see him in the New Year.
[Update March 2010]
As previously reported, in December 2009, my PSA was 0.1 (not "less than 0.1" as it had been since my surgery) - so my GP suggested another test in 3 months and to make an appointment with my Urologist. (I haven't actually seen my Urologist since November 2005 - before that I was phoning his nurse for the results.) and then by arrangement PSA was added to all my other annual blood tests and my GP would give me the result.
I have just returned from seeing my urologist and my PSA is again 0.1 (not "less than 0.1"). He says he's not worried by two "0.1" readings in 3 months but as a precaution suggested another blood test in 6 months. But after telling him that Pam and I were planning to leave end of May on a caravan trip to WA for 5 months he was OK with a blood test before we go.
He says the likely scenarios are:
(1) if it's again 0.1, then another test in 6 months;
(2) if it rises to 0.2, then a test in 3 months while we are away and phone for the result;
(3) if it gradually rises to 0.4 or 0.5 he would start radiotherapy immediately; but then,
(4) it is quite possible it may return to less than 0.10.
Had another PSA test on 7th May and the result was again 0.1 - Next check in December so we are off soon to Western Australia in the caravan.
Back from another adventure, and planning the next one - small ship cruise, this time Iceland followed by a self driving tour of Scandinavia, Eric had a spot of time to get his PSA checked and has this to say:
I had another PSA test earlier this week and phoned the urologist's nurse for the result yesterday. She said it was "Perfect" without actually giving me the result. When I asked she said "0.1" (not < 0.1) and then asked if I wanted to keep my appointment to which I said "No, unless you think it's necessary." She said "no" but would make an appointment for six month's time.
If there is anyone who epitomises the aspect of "There Is Life After PCa" it is Eric, I reckon.
With three weeks to go before his next Odyssey, Eric mailed me to say:
Just phoned for my latest PSA test result and it was 0.10 again. It's been the same now since Dec 2009 so I have cancelled an appointment with my urologist (made 6 months ago by his nurse - "just in case….").
I will have another PSA check in six months but if that's the same I will discuss with him going back to annual tests to coincide with my annual check up with my GP.
I have just had my 6 monthly PSA test and the figure is now "0.12" ........ so, from - "less than 0.1" in Dec 2000 (after surgery) - to "0.1" in Dec. 2009 - to "0.12" Dec 2011 a rise of 0.02! Why is it so?
My urologist said that Pathology is now reporting PSA to 2 decimals places. So it could have been "0.12" back in Dec 2009 - who knows? [I think that the most likely reason behind Eric's change in PSA numbers is a change at the pathology laboratory which may well have switched from normal PSA testing to Ultrasensitive or even Third Generation tests. It is always worth getting copies of a PSA report and checking to see if there has been a change.] But he's not concerned saying, "the number is less important than the time it takes to get there" (and in my case that's 11 years). He said it is (quote) 'exquisitely' (unquote) unlikely that it will rise dramatically but if and when it does rise again it will probably be in small increments over a long period of time at which time he may consider suggesting radiation then hormone treatment".
Given the probably side effects of those treatments, I think I would need a lot of convincing. Interesting forecast given that medical professionals are reluctant to give predictions and given he said in Nov. 2005 "..... it's very rare that PSA has been known to rise after 5 years - post operation but after 10 years it has not occurred to my knowledge". As I've said before if he's not worried, why should I be?
Next test June 2012.
June 2012 - 12 years post Op :-)
I phoned my Urologist's nurse for latest PSA and was informed it is 0.1 "What about the second number?", I asked and in summary she replied, ".... Your PSA is actually 0.16 (previously was 0.12) .... but don't worry about the second decimal place, next time it could be down a bit, it is not significant and not normally used to consider a change to a patient's treatment......we don't even say "less than" (eg. <0.1) any more as miniscule increases causes unnecessary anxiety amongst our patients. [There seems to be some kind of informal agreement among doctors on this issue. As Mike C reported some months ago, his doctor in Canada has said the same thing. There was a recent study on this issue and you can see it at Ultra-sensitive PSA]
Next check December 2012.
I got the result of my latest PSA today , 6 months ago = 0.16. today = 0.29 Urologist says he's OK with that and will do another test in 6 months.
A church friend of mine had the 'op' about 4.5 years ago, PSA stayed less than 0.1 for a couple of years and then gradually rose 0.27 earlier this year. His/my urologist (one and the same) suggested he see an Oncologist and he underwent radiation. Why him and not me? Perhaps his PSA rose in 4 years where mine only after 10 years?
Here are two of several 'sayings' I have picked up over the years and use occasionally when speaking to other people - but I also try to apply them to myself:-
(1) Never die wondering..." ie. if in doubt, check it out.
(or as Kelly Exeter's blog says, "life is way too short for regrets and 'what ifs' ")
and
(2) Hope (and pray) for the best but prepare for the worst.
After the last PSA result of 0.29, I was encouraged, via email from 'Paul M B' who had read my story, to be tested again soon. He concluded with, "...for God's sake don't wait half a year!?
Isn't is wonderful when someone is worried about others they've never met. I really appreciated his concern so I said I would get tested a bit earlier - in March. I guess you could say, I partially ignored the first 'saying' - but as I've said before, '.. If my urologisy wasn't worried, why should I be..' - but true to form, my GP (general practitioner/family doctor) was concerned. During my recent annual check up while reviewing the results of various blood tests he decided to override my Urologist and ordered a PSA test immediately along with the usual numerous other blood tests he requests at least annually. As usual, he asked me to call him in a few days for the results. Believe me, I was definitely not ignoring the second 'saying' when I dialed his number.
When he finally came to the PSA result he said, " It's come down! from 0.29 to 0.19.." but as cautious as ever he also said I should be tested again in May as per the Urologist request. This I will do. with 'bated' breath :-)
Well, my Urologist has decided my next PSA test should be late September 2013 :)
24th September 2103
Latest result is 0.2. (Note: No 2nd decimal place any more). Have just returned from a 4 month's caravan holiday to Darwin via Cooktown and returning via central Queensland & NSW - 16,600kms.
Next check up in 6 months time.
Visited by GP today for a flu and pneumonia shots. He had received latest PSA (sample taken yesterday) which he said was 0.48 this is after staying at less than 0.1 for 10 years. It's been creeping up since then to 0.29 but it did drop once to 0.16. So I called my Urologist's nurse who said it was 0.4 (doesn't give 2nd decimal place) and suggested I keep my appointment next Tuesday as I had not seen him (only because he didn't previously see the need to see me) for two years. More after next Tuesday :-)
In October 2005 my PSA remained at less than 0.10 ng/ml. My Urologist said then, "it's very rare that PSA has been known to rise 5 years post Op. but after 10 years it has not occurred" to his knowledge". I visited my Urologist yesterday who said he doesn't say that any more. Over the past few years PSA of patients of his and his colleagues has been rising - so what's changed to make this happen?
My PSA has risen from 0.29 to 0.48 which my Urologist says is not due to the Total Ankle Replacement Op. (due to arthritis and cartilage damage) I had on 12th March. He has recommended that, as I have no other health issues, I talk to an Oncologist, "Now". Having reasoned later to myself that 'short term pain' (of Op. and recovery) would result in 'long term gain' for my ankle, to me, the same reasoning may apply to Radiation so I will see an Oncologist then consider my options.
On 24th April, Pam & I met with an Oncologist and his female Registrar at Wollongong Hospital Cancer Care Centre for a very relaxed and unhurried information, Q & A session - In fact we were very impressed how it all went as they were both very pleasant people to converse with. The Oncologist said, given my general good health and relatively low PSA, the cancer cells 'should' still confined the Prostate 'bed' and Radiotherapy has a 50-60% chance of eliminating them - but no guarantees! I was surprised he was prepared to quote a %-age but with those 'odds' I am going ahead with the treatment. A "Planning" session is on 1st May and treatment follows maybe 2 weeks after that. I know what will happen if I do nothing - so to go along with 'one' of my favourite sayings, ie. "Don't die wondering...." , I am doing something knowing it may help or may just delay things...........
On 8th April my PSA was 0.48 and on 15th May it had dropped to 0.36. However, my GP, Oncologist and Urologist all advised to start Radiotherapy which I did on Monday 2nd June and will have a total of 33 treatments - one is done each weekday (M-F). After 19 treatments I saw a Cancer Centre doctor for minor issues with bowel movement which could have resulted from either (1) a complete change in diet before the treatment started from a High Fibre (to manage slightly elevated Cholesterol) to a Low Fibre diet (saw a dietitian for this), (2) Magnesium Tablets (mild laxative & to manage 'gas') and/or (3) Radiotherapy. I am feeling a bit tired in the afternoon but perhaps no more than usual for a 70 year old :-)
I saw the Oncologist today and my PSA is now 0.24 down from 0.36 in May 2014 - not quite the result the Oncologist was hoping for but as he said it's early days and my PSA will be checked again in 6 months at which time the effects of the Radiotherapy on the cancer cells will be complete. Apparently, Radiotherapy damages the DNA in the cancer cells and the amount of damage determines whether the cancer cells will die (PSA reduces) or they reproduce (PSA increases) in which case a body scan will determine where these cells are. If the PSA increases, the rate of increase will determine if and when a treatment (eg. hormones) will be recommended. The Oncologist is not greatly concerned as it seems I am one of his more 'healthy' patients. As he said, "don't worry about the PSA numbers, just get on with life" which we always intended to do anyway.
Just a quick update - before Radiotherapy = 0.36, 6 weeks after Radiotherapy = 0.24 and the latest (15 Dec today) = 0.14 - so still going down. Next test March 2015.
I saw my Oncologist today (24th March 2015) who said there is currently no evidence of prostate cancer - my current PSA is 0.09 which could still go down further. I had been offered a Gallium 68 PSMA* body scan at Royal Brisbane Hospital but my Oncologist says it's not required unless my PSA starts to rise again rapidly.
* A study "Comparison of PET imaging with a 68Ga-labelled PSMA ligand and 18F-choline-based PET/CT for the diagnosis of recurrent prostate cancer" concluded that Positron emission tomography (PET) using Gallium 68 PSMA (prostate-specific membrane antigen) - "detects PC relapses and metastases with significantly improved contrast when compared to choline-based PET/CT. Nevertheless, the most significant advantages of 68Ga-PSMA PET/CTare the sensitive detection of lesions even at low PSA levels, of even small lymph node metastases (primarily due to a high radiotracer uptake) and of central bone and liver metastases due to low background signal."
Latest PSA is 0.12 up from 0.09 in March 2015. The Oncologist's Registrar says it may be no more than a "flicker" but will test again in December to see where it is trending.
Not related but may be of interest: (a) Very little discomfort now with my Total Left Ankle Replacement which was done March 2014. (b) Findings of a recent MRI performed due to pain in upper legs suggests cause may be due to moderate to severe central canal Stenosis. A report following a Whole body bone scan says elsewhere whole body images do NOT demonstrate any features to suggest metastatic disease.
Otherwise feeling great as have just returned from a 3 month's holiday in our caravan covering over 11,000 Kms around the central parts of Australia.
Latest PSA is 0.23 up from 0.12 in October - apparently still a bit too low to consider a PSMA PET CT scan at this stage. Next test in March 2106.
My PSA as at 18th March is 0.19 down a bit from December 2015. My Oncologist discuss "PET" scans (now available in Sydney) but recommends against it until my PSA is at least 1.0.
Recently sold our house and now living in our 13' caravan until our Villa in a new Retirement Complex is ready - expected completion - early 2017.
My PSA test result today 2nd Sept 2016 was 0.13. My Oncologist was pleased with the result [so was I :-) ] saying it normally takes 18-24 month after Radiotherapy for PSA to level out and so 0.13 may be my new base level.
We are still living in our 13' caravan but doing quite a bit of house-sitting for friends and family.
The latest update on moving into our new retirement villa at Shell Cove NSW is now May/June 2017. The new retirement complex will consist of 33 self care villas, 47 self care apartments (3 story building) and 127 room Residential Care complex occupying levels 2 & 3 of a 3 story building. All except the apartments (they will commence building those in a few months) need to be completed before anyone can move in.
I saw my Oncologist on Friday 3rd March 2017 and my PSA has risen from 0.13 to 0.14. He had no cause for concern so neither have I :) ha ha. Again he suggested this may be my new baseline.
PSA is now 0.23 up from 0.14 last March but my Oncologist is not concerned "a baseline fluctuation perhaps and still too low for a PET scan or new treatment that may be necessary 10 years (maybe 5)". He asked how I was generally feeling and I said "great, why?" (I thought he had found something else in the blood test). He said I noticed you are just on thyroid and cholesterol tablets - far less general medication than most guys I see of a similar age.
An update on our 3 bedroom 150 sq metre Retirement Villa: after a couple more delays our official "move in" date is 20th Sept - it is just 1/2 km from a new marina being built at Shell Cove NSW.
But I find I am far less anxious about these PSA tests these days. Why? I know my "heavenly home" is secure.
I was due to meet with my Oncologist on Friday 16th March 2018 but instead he called and left a voicemail saying, "Sorry I can't meet you today. Your latest PSA s 0.28 which is excellent". Our caravan trips are over as we have sold it - now exploring new types of holidays :)
My PSA (as at 26th Sept) was 0.5 up from 0.28. But my Oncologist is still not concerned - so neither am I :-) He seems to think the latest PSA indicates that perhaps the cancer may have spread to lymph nodes but not the bones. If/when PSA = 1.0, he will recommend a GaPSMA PET scan which is available at Liverpool Hospital (100km away).
Just clocked up 12 months in our Community Village Villa and recently enjoyed a trip to Guernsey (Channel Islands UK).
As at 5th February 2019, my was 0.49, ie. down from 0.52 in September 2018 but up from 0.28 in March 2018 so it was going in the wrong direction.
My GP said my PSA had dropped a bit - better than "Up". However, my Oncologist, who was expecting it to rise again because he ordered a PSA test be done 2 months earlier than normal, said my PSA "had stabilised" and "we don't need to do anything but monitor it again in August 2019", ie. back to 6 monthly checks.
So what's in a number? I am 75, it's been 19 years since being diagnosed and feel great. OK, I generally have a nap most afternoons
My nephew is a Principal Radiochemist tells me that tests are now being carried out on a new capsule which will not only find where the cancer is (currently used in GaPSMA PET scan) but will eventually neutalised it;
Yesterday, 7th August 2019, my PSA was 0.61 (5th February 2019 = 0.49, September 2018 = 0.52 and March 2018 = 0.28).
My Oncologist again considered requesting a PET Scan but again decided to leave it until PSA gets to 1.0 when it would be more reliable. He was thinking of sending me to Liverpool because although money has been allocated for a machine at Wollongong Hospital is still hasn't been ordered.
Next check on my PSA will be 27th November 2019.
My PSA today (7th November 2019) was 0.76 up from 0.61 in August. A slow rise so my Oncologist is still not too worried but has requested another blood test on 18th March 2020 at which time he may request a PET Scan regardless of the result. My general health is good and I am still enjoying life :-)
Time Line
- July 2000: Diagnosed with PCa: 7.00 ng/ml, Gleason Score was 9, stage T1c.
- October 2000: Prostatectomy after which the cancer was "undetectable" for 9 years .... then my PSA started to slowly rise again.
- June 2014: Started 33 treatments of Radiotherapy
- March 2015: PSA was again undetectable.
- March 2016: PSA fluctuating. Oncologist Dr Nasser suggests when PSA = 1.0 he will request a PET Scan
- March 2017: PSA on the rise again
- March 2020: After fluctuating but trending upwards, PSA is now 1.1 . PET Scan (Google it
 ) requested for June 2020 at RPA Hospital Sydney where my nephew Stehen Taylor is a Principal Scientist. He tells me I will be injected with a radio isotype substance which will detect where the cancer is in my body and display it as a 3D image on a screen for analysis and a decision on best next treatment.
) requested for June 2020 at RPA Hospital Sydney where my nephew Stehen Taylor is a Principal Scientist. He tells me I will be injected with a radio isotype substance which will detect where the cancer is in my body and display it as a 3D image on a screen for analysis and a decision on best next treatment.
This latest development doesn't worry me because I know PCa is slow growing and Dr Nasser whom I trust implicitly is looking after me which means, with his treatment and as a Christian, I am likely to go to heaven 'with' PCa rather than 'because' of it 

Hi All
- August 2000 (20 Years ago) I was diagnosed with Prostate Cancer, my PSA = 7 Gleason = 9 and I choose surgery (Perineal Prostatectomy) which was performed October 2000.
- April 2014 my PSA= 0.48 and in June 2014 started Radiotherapy
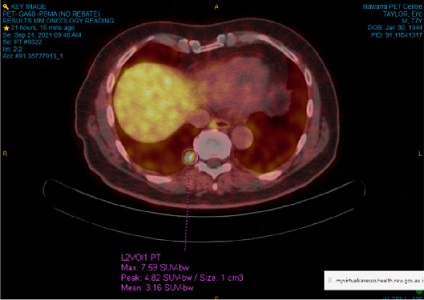
- April 2020 my PSA = 1.1 and my Oncologist suggested a Whole Body 68-Gallium PSMA PET-CT Scan at Royal Prince Alfred (where Stephen is Principal Scientist - Radio-Chemistry).
This scan was done on 7th May and detected that the radioactive tracer had been taken up by just one 8 mm nodule which was verified by a subsequent Pelvis Scan on 26th May. - At a Multidiscipline Medical Team Meeting of (Oncologists, Urologist, etc, on 3rd June 2020 the consensus was to go with Surgery but "do nothing, for a while" and Radiotherapy were options.
- This Thursday 11th June 2020 will having Robot Assisted Surgery for the removal of that one 8mm nodule and free my body of cancer forever, but no guarantees
I saw my Urologist/Surgeon yesterday (24th June) for a chat following recent Robotic Assisted surgery remove a suspected an 8mm Tumour adjacent to the right side of my Bladder which was picked up in a Whole Body 68-Gallium PSMA PET-CT Scan performed on 7th May 2020.
Surgery:
Was on 11th June 2020 from 8am -11.30amafter which my Urologist/Surgeon called my wife to say surgery went well and there was no bleeding. It was great he did that because I had my usual issues waking up after Anaesthetic and couldn't call her until next morning
Pathology Results
- Prostate Cancer detected in the removed 8mm Tumour.
- No Cancer in the tissue removed above and below the tumour and up to adjacent the bone.
- No Cancer in the seven Lymph Nodes surrounding the Tumour that were removed.
A very welcome result following a prostatechomy 20 years ago following by Radiotherapy 6 years ago
MY PSA before surgery was 1.1. Next PSA Test: 5th August 2020
Options if cancer re-appears are:
- Radiotherapy depending on location of the cancer. OK with that
- Hormone Treatment. Mmmm
Well today 5th August 2020, my Urologist/Surgeon in a phone consultation said: -
- my PSA was now 0.89 ...... which wasn't as low as he thought it would be after he removed an 8mm tumour, some tissue and 7 lymph nodes on 11th June;
- indicates there is still some very small cancer cells still lurking in my body which wasn't picked up in the PET scan;
- PSA is stiil very low so he doesn't expect cancer should trouble me for at least 10 years;
- Pathology Lab didn't give him a revised Gleason Score (which twenty years ago at initial diagnisis was "9" then and revised down to "7" after Prostate was removed) …… but he will now ask for it again; and
- He had already spoken to my Oncologist who will continue to monitor my PSA for now on .... next test in 6 weeks time............
My latest PSA is 0.95 up from 0.89 in August. Dr Nasser, my Oncologist says there is obviously still some cancer cells in my body which were too small to be detected by my PET-CT Scan in April. He is scheduling another PSA test for December and if the result is more than 2.0 ng/mL he will request another Whole Body 68-Gallium PSMA PET-CT Scan.
PSA result received today 11th December 2020 was 1.2 ng/mL a slight rise from 0.95 in Septemaber 2020 and up from 0.89 in August 2020. Plan remains the same, ie. when PSA = 2.0 ng/mL my Oncologist will request another Whole Body 68-Gallium PSMA PET-CT Scan.
Due to the COVOD-19 Pandamic, since March 2020 I have been having Phone Consultations with my Oncologist Dr Nasser. On 11th March 2021, he said my PSA with 1.3 ng/mL up from 1.2 last December.
He is still recommending that when my PSA reaches 2.0 ng/mL he will request another Whole Body 68-Gallium PSMA PET-CT Scan to see where the cancer cells are now and if the ones that weren't visable (but clearly there) back in June 2020 have grown and can ne removed by an operation or Radiotherapy.
For the past 12 months or so, when I should be sleeping, I have been going to the toilet quite a bit sometime almost every hour! So on 1st March, I talked (face to face) my Uroogist Dr Chin who said Alcohol and Caffeine can be a problem and so I have switched to Decaffeinated tea (2 per day) and coffee (2 per day), I still have one glass of wine with Dinner :-).
He prescibed Betmiga (containing Mirabegron) which is used to treat symptoms of an overactive bladder and requested I start a "Bladder Diary" to record my Bed times/Wake times, every amount of Liquid intake and Urine Output and "bladder sensations". The trips to the loo has reduced to 2 - 3 per night. I see Dr Chin again on the 14th April.
I received an pre-arranged call yesterday from the Registrar my local Cancer Clinic. She advised me that my Prostate-Specific Antigen (PSA) had increased from 1.3 ng/mL in March 2021 to 3.2 ng/mL on 10th August 2021 and will arrange for me to see my Oncologist within the next few weeks to discuss my options which should include another PSA Test (to confirm the one just done) and a complete body PET scan to see where the cancer is and the size of the cancer cells.
I think my options will be more Surgery or Radiotherapy… but I will let you know what my Oncologist suggests and what I choose.
In the meanrime, it was with a sigh of relief that a few weeks ago I received my 2nd AstraZenica vaccination. Despite the best efforts of the NSW (Australia) State Government, people continue to disobey the "Total Lockdown" rules (now NSW State wide), to stay at home, resulting in the Delta strain of COVID-19 virus which is much more contagious being spread to anyone close by without a mask and causing both younger and older people to die if not vaccinated.
I thought I should let you know where I am at with my battle with Prostate Cancer since August 2000 when I was first diagnosed. It's been a roller coaster ride then:-
- Sept 2000 - Before Prostatectomy my PSA was 7.0 and anything of 4.0 is a concern. After PSA went down to less than 0.1 (technically undetectable)
- 2014 - PSA had risen to 0.45 and Radiotherapy was commenced after which my PSA dropped to less than 0.1
- May 2020 - PSA has risen to 1.2 and after surgery to remove an 8mm tumour my PSA drop only to 0.89
- July 2021 - PSA rose from 1.2 to 3.3 four months and so my Oncologist Dr Nasser ordered a PSMA Pet Scan on Monday, Sept 20. to see where the cancer is and further treatment options.
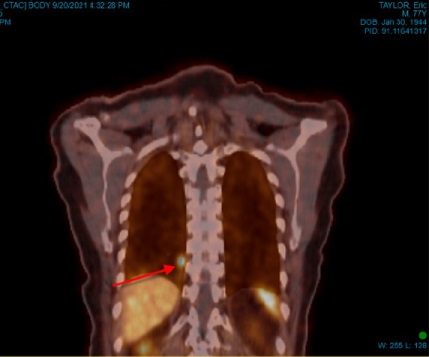
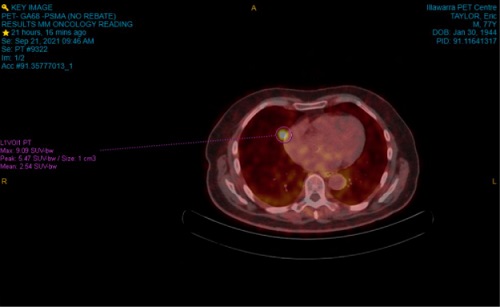
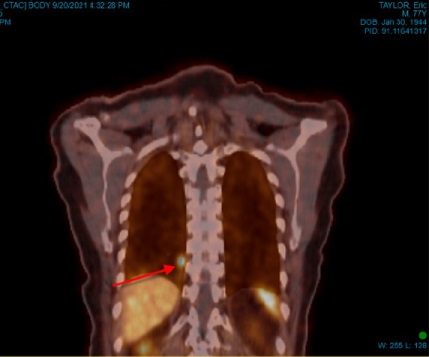
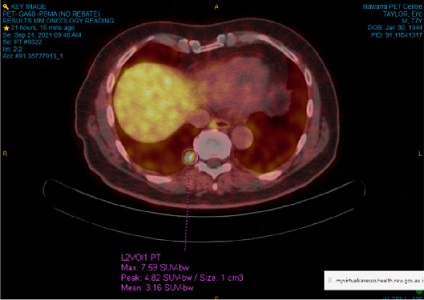
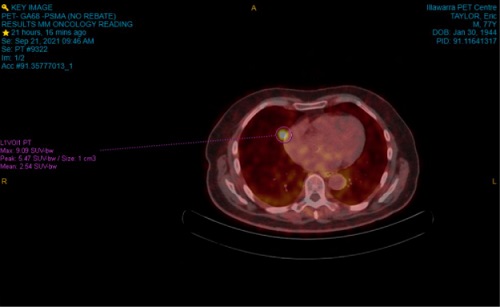
All went well with the CT Scan and then the PET Scan from my skull to mid femora and I was at Wollongong Hospital PET Centre from 2 - 5pm.
On Tuesday there was an online chat between Dr Nasser, Pam and I. Below are the results of the Scans and Treatment options.
Findings:
- No tumours/nodules in Pelvis area. (If tumour is less than 3 cm (30mm) in diameter, it's commonly called a nodule)
- 1 x 6 x 8mm Nodule in/on the Lung, near Heart.
- 1 x 7mm Nodule near the Vertebral Column.
- Liver image is bright on scan but not PC related.

Treatments options: Hormone Treatment or Radiotherapy. Surgery is not an option due to nodule locations particularly near lung/heart.
I have agreed to 3-4 weeks of Radiotherapy which will start in 3-4 weeks. The Radiotherapy “Planning” session is on 29th Sept and then the actual treatment starts a week after that.
Seven years ago in May 2014 my PSA was 0.48. Radiotherapy was recommended and after 33 Treatments my PSA initially dropped to 0.36 and then after 6 months eventually dropped to 0.09.
In September 2021 my PSA was 3.3. Following 15 days of Radiotherapy, my Oncologist recommended at least 6 weeks before another blood test which I had just a few days ago. This was followed with an “online” appointment on 23rd December when my Oncologist briefly appeared on camera behind the Cliincian but didn’t say anything just gave me a “Thumbs UP. Then my Clinician said my PSA was now 1.9 down from 3.3 which while heading in the right direction, to me was a little disappointing, but I am otherwise generally in good health.
Later in our chat my Clinician said just like in 2014 my PSA should come down more when I have my next Blood Test 22nd April 2022.
Today’s PSA was 2.8, ie. up from 1.9 in December 2021 following Radiotherapy …..unfortunately not the direction my Clinician said it could go.
Next PSA test will be October 2022
I now have new Oncologist: Dr Natalie Collier at the Illawarra Cancer Care Centre in Wollongong NSW. Dr Collier replaces my previous Oncologist Dr Elias Nasser who has decided to become a GP in a town somewhere in Western NSW.
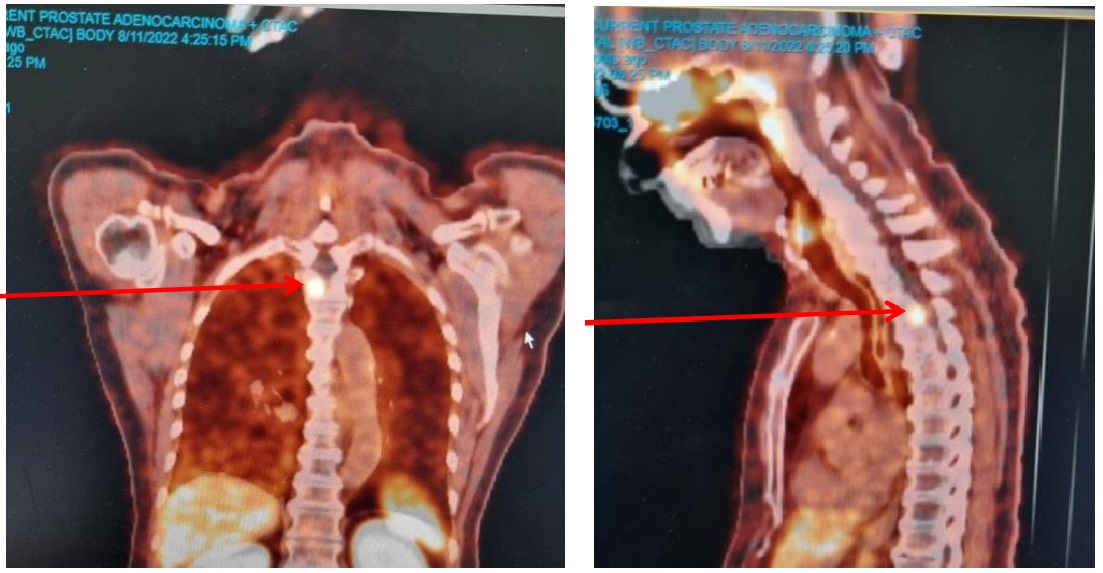
Prior to phone consultation with Dr Collier on 22nd July, she requested the usual PSA blood text and a CT scan with contast of the chest, abdomen and pelvis to determine if the cancer had metastasised (spread) to my bones. My new PSA is now 4.8 up from 2.8, indicating that some small cancer nodules were in my tissue but there was none in my bones.
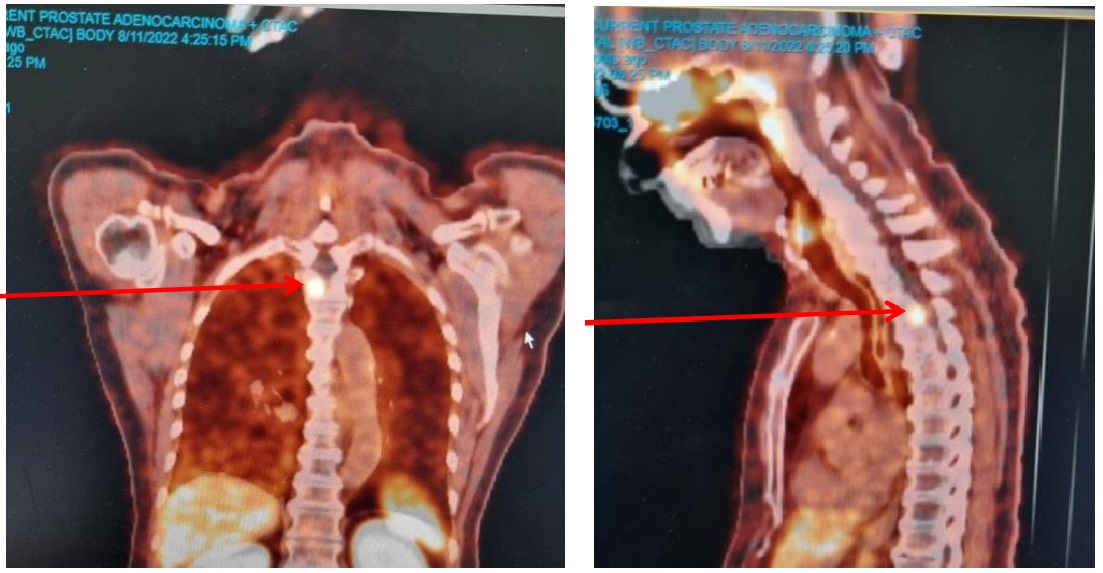
I had a PET/PSMA scan on 11th August and it showed a 13mm tumour in my spine - below my collar bone, mid shoulder blade Level. Following some discussion with my oncologist, I will be having another 15 sessions of Radiotherapy (as I had in November 2021) in a few weeks’ time.
I was also offered "Stereotactic Body Radiation Therapy" (SBRT) which delivers higher doses on Radiation requiring only two sessions. However it can only be performed in a couple of Sydney Hospitals and at a cost to me.
So Hormone treatment will be delayed for now
My PSA has risen from 5.6 to 9.0. My Oncologist is still suggesting Hormone treatment as my best option. But first I will have a CT scan of my Chest, Abdomen and Pelvis and a WBBS - Whole Body Bone Scan. Depending on what that shows I will have another PSMA scan. I will see my Oncologist again on 31st March to obtain the results and discuss options.
I had an appointment with my Oncologist today for the results of the recent CT scan of my chest, abdomen and pelvis and a whole body bone scan. Even though my PSA has risen from 5.6 to 9.0 …… no new tumours showed up. Oncologist said after treatment for some unknown reason there could be a “bounce” in the PSA number but then it should fall. I am to have another PSA blood test in about a month to see what’s happening and that may be followed by a PET (PSMA) Scan.
My PSA is now 9.9 up from 9.0 in March. The test was done to see if a posible PSA "bounce" occured following Radiotherapy late last year. My Onchologist has agreed to another PSMA test to see where the tumours are and how large they are.
On 3rd May 2023, my PSA was 9.9 so on 30th May, I had another PSMA Scan which showed previous Radiation Treatments to T3 (spine) and Lung that the Lesions are fading. However, new 4 spots were visible in the right lung in the Pleura (lining of Lung). My Radiation Oncologist has recommended a higher resolution CT scan, that I begin Hormone Treatment prescribing “Firmagon” and “Lucrin” (injections) and has referred me to a Medical Oncologist.
Last month, my Radiotherapy Oncologist advised me that there was no more Radiotherapy could be done and recommended I start on Hormone Treatment.
On Wednesday 19th July 2023, my wife and I met with my Medical Oncologist Team: firstly with the Registrar and then the Doctor.
I was delighted to learn that following just 2 injectons of Firmagon on 16th June (one each side of stomach), my PSA had fallen from 9.9 to 0.28.
Side effects so far have been Hot Flushes, Fatigue. However, with doing my morning physiotherapy exercises and later an hour of walking, my weight has reduced from 77.3kg 26th June to 75.6kg 15th July.
The Team recommended I start taking Apalutamide tablets which will assist in controlling the Cancer. Starting Chemotherapy was a third option but that will not be implemented at this stage.
On 17th July, I had one injection of Lucrin ..... this will be taken every 3 months from now on.
On 21st July I started taking Apalutamide.
I will be meeting with Medical Oncologist Team again on 16th August.
At my second appointment with my Medical Oncologist) on 16th August he advised :-
- My PSA had dropped again from 0.28 to 0.02; and
- I should increase the Apalutamide tablets from 2 to 3 tablets per day.
- I am in remission for now, however the cancer is "smart" and can find its way around the medication resulting in my PSA slowly rising again at which time he would look for an alternative treatment.
I am feeling the Side effects of Hot Flushes for which I have medication and Fatigue but still managing to do my exercises and up to 1 hour walk most days.
13th September, I saw Dr Kasherman (Medical Oncologist) and told him the side effects I was experiencing and he said they were unacceptable, affecting my quality of life. However, he said there was some new hormone medication available which claimed to have far less side effects. So, I am now on Abiraterone (Hormone treatment), Prednisolone (Steroids) and Oxybutynin (for hot flushes).
I saw him again 11th October he said my PSA is now 0.01 and I said the side effects, ie. Brain Fog, Fatigue and hot Flushes were much less.
Eric's e-mail address is: outback21 AT bigpond.com (replace "AT" with "@")




 ) requested for June 2020 at RPA Hospital Sydney where my nephew Stehen Taylor is a Principal Scientist. He tells me I will be injected with a radio isotype substance which will detect where the cancer is in my body and display it as a 3D image on a screen for analysis and a decision on best next treatment.
) requested for June 2020 at RPA Hospital Sydney where my nephew Stehen Taylor is a Principal Scientist. He tells me I will be injected with a radio isotype substance which will detect where the cancer is in my body and display it as a 3D image on a screen for analysis and a decision on best next treatment.