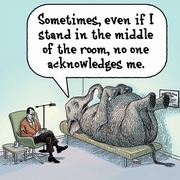
 THE ELEPHANT IN THE ROOM
THE ELEPHANT IN THE ROOM
The
Elephant In The Room as far as prostate cancer is concerned is anything to do
with death or dying. The subject rarely comes up on Lists or Forums and if it
does is greeted with a hushed silence. Yet it is the main driver behind all decisions
to do with the disease - people want to know "How long have I got?" "How does
death come?" So here's my take, modified by some excellent input after the subject
was discussed on the Lists.
HOW LONG HAVE I GOT?
There is
no definitive resolution to this question because there are so many variables.
Many doctors avoid the issue, if they can, because it is such a difficult enquiry
to answer. If they do respond, the question and answer that is remembered by the
patient may not 'match' what the doctor said. Patients will often qualify the
question by asking "How long have I got? What is the worst case, doctor?"
The doctor's answer may be that although some men with advanced prostate cancer
may only live three to five years; that most men, even men with aggressive disease
will live for many years; that the actual outcome depends on many factors; and
so on. But what the questioner remembers is "Three to five years."
Some
of the issues that have a bearing on the answer to the question are summarised
below.
1.
The diagnosis.
There
are significant differences in the likely outcome in the range of different diagnoses
that can be made for what is not a simple 'one size fits all' disease. There are
many variances in the disease itself.
A
"bad" diagnosis will generally be associated with a high Gleason Score
of 8, 9 or 10; a history of sharply rising PSA numbers; a low free PSA percentage
(under 15%); a high PSA level, well over 20 ng/ml and probably in the hundreds;
a staging of T3 or T4. Such a diagnosis carries a high, but not a 100%, chance
of early rather than late death.
At
the other end of the range is the "good" diagnosis typified by a Gleason
Score of 6 or less; a history of small or increments in PSA levels; a high free
PSA percentage (over 25%); a PSA level below 10 ng/ml; a staging of T1. Such a
diagnosis carries a very low, but not a zero, risk of disease specific death.
These
diagnostic items are variable - for example there is a very dangerous form of
the disease that has a low PSA level and is often only diagnosed late in the day
through DRE (Digital Rectal Examination) or the development of symptoms because
the PSA levels generated never hit any of the current trip wires. Recent studies
have identified 24 genetic variants of the disease which may help to identify
the aggresiveness of the specific variant of disease which has been diagnosed.
An article in the Wall Street Journal covers this work - see The
Prostate Cancer Quandry.
2.
Age at diagnosis.
The
SEER statistics for the USA 2002-2006 show the median age at diagnosis for prostate
cancer was 68 years of age. Approximately 0.60% men were diagnosed aged between
35 and 44; 8.7% between 45 and 54; 29.0% between 55 and 64; 35.6% between 65 and
74; 21.4% between 75 and 84; and 4.7% 85+ years of age. This is about 7 years
younger than it was prior to the introduction of PSA tests, when the median age
was in the mid-70s.
The
latest SEER mortality rates (2002-2006) show the median age at death for cancer
of the prostate was 80 years of age. That is to say, half the men who died from
prostate cancer during this period were more than 80 years of age. The figures
also show that over 90% of the men who died were over the age of 65. There were
no statistically valid deaths for men under the age of 34 and between 35 and 64
these were the relevant figures: 0.1% between 35 and 44; 1.4% between 45 and 54;
7.2% between 55 and 64.
There
is a view that any diagnosed disease in a young man is more aggressive, but this
is not supported by available data and arises from the pre-PSA era when very few
young men - men in their 40s and 50s - were diagnosed.
3.
Other causes of death:
Overall,
despite the statements in publicity material, prostate cancer is not a major killer
of men. In most Western countries, such deaths account for only about 3% of male
deaths; in countries with lower life expectancies prostate cancer often does not
feature on the mortality tables because men in those countries simply do not live
long enough.
The
mortality rate for men diagnosed with prostate cancer is higher than the overall,
national rate, but, generally speaking, men with PCa still have a higher risk
of dying from some cause other than this disease. Two recent studies illustrate
this point fairly clearly.
The
first, published
in 2008 was a fairly large one with a population-based cohort study of 19,271
men aged 66 years or older diagnosed with clinical stage T1-T2 prostate cancer.
Some (41%) of these men had ADT (Androgen Deprivation Therapy); others were watched
for progression. During the follow-up period (the median follow up time was 81
months, a little under 7 years) almost two thirds of the men died - 11 045 (88%)
of all deaths were from causes other than PCa and 1560 (8% of the men in the study)
from prostate cancer.
The
second
study is an ongoing one on Active Surveillance, results for which were presented
in May 2009 at the AUA conference. The median follow-up in this study, which is
a smaller one with only 453 is 7.2 years. In that time 17% of the men in the study
have died with 5 men (1%) of the men in the study, dying from prostate cancer.
The ratio of non-prostate cancer to prostate cancer mortality was 16:1. The men
in this study had diagnoses very close to the "good" diagnosis set out above.
None
of these three factors can, in themselves, produce a firm answer to the question
"How long have I got?" but taken together they can help to give an indication
of the potential survival time for an individual, who can assess where his diagnosis
fits into the range; how old he is; what his general state of health is and what
his activities are. Hopefully in completing this exercise he will come to the
conclusion that he has many years ahead of him and that he can fully realise that
there is indeed life after Prostate Cancer and to realise that this is still primarily
a disease of old men, at least as far as death is concerned. As Willet Whitmore
said, many years ago: "Growing old is invariably fatal while prostate
cancer is only sometimes so".
HOW DOES DEATH COME?
For
most people, the word "cancer" is an emotionally laden one, and I was no exception
to this rule when I was diagnosed. It is usually associated with a drawn out,
painful death and this is particularly so as far as prostate cancer is concerned,
where metastasis to the bone can create significant pain.
There is no
doubt that this can, and does happen in a significant number of men and it is
an awful fate for them and their loved ones, but the two most common causes of
death associated with prostate cancer are cardiovascular and respiratory failure
- heart attacks and pneumonia. In the few discussions that have occurred, experts
in the field of prostate cancer have said that modern pain management techniques
can deal with most of the issues and that, in any event, the dreaded painful bony
metastasis is less common than imagined, at least in their experience. I know
of no studies that try to evaluate the issue of pain associated with metastasis
to the bone, but it seems clear that not all such events are painful. Jacquie
Strax, who publishes the excellent PSA Rising site has a page with more information
on the subject of Pain
Control for Cancer Patients and there is a good page in the Prostate
Charity Toolbox.
I
recently came across a piece written by Dr. Michael Glode on his blog
in October 2007 where he answers the question, How does prostate cancer
actually kill you? He says in part:
Prostate cancer tends to spread
to lymph nodes or bones. There are some studies that begin to show us why this
is different in different patients ……. but have yet to lead to more practical
management decisions.
[One
study shows the situation of the 10 most common metastases discovered in post
mortem examinations as Bone: 90%; Lung: 46%; Liver: 25%; Pleura: 21%; Adrenal
Gland: 13%; Brain and Meninges: 7.5%; Peritoneum: 7.0%; Ureter/urethra: 3.4%;
Kidney: 3.1%; Pericardium: 2.5%. The percentages add up to more than 100% because
there are usauly multiple sites.]
We
treat all metastases first with androgen deprivation. In those patients with nodes,
we ….. ..keep the ureters open as they may be compressed by the enlarging nodes.
Without these interventions, the kidneys can stop working and lead to death from
accumulation of toxins normally excreted in the urine.
For
those patients in whom bone metastases dominate, the main issue is often pain
management. Radiation to bones that have tumor deposits can be extremely helpful
along with appropriate pain medications. It is highly unusual to have a patient
in whom pain cannot be well controlled with radiation, opiates, NSAIDs and attentive
care.
This
is certainly reflected in my personal experience of friends who have died from
this disease and when I posted this piece on the Web, this was one of the responses:
I
am a hospice social worker who was diagnosed with prostate cancer in 2005. So
I have two perspectives on the disease, as a survivor and as individual who has
provided counseling, emotional support, education and advocacy to patients dying
from prostate cancer. The focus of hospice is to maximize a patient's quality
of life while assisting him/her with the transition from this life. Prostate cancer
patients generally enter a hospice program when they have six months or less to
survive. The majority of PC patients who have died under my agency's care went
peacefully with a minimal amount of physical pain and emotional stress.
Dame
Cicely Saunders is regarded as the founder of the modern hospice movement,
opening St. Christopher's hospice in 1967. As a nurse, she knew that, as she said,
"dying is hard work" and she transformed the way we look at death and dying, ridiculing
some of the medical profession for not giving large doses of pain-killing drugs
on the grounds that they might become addictive. If the patient were dying anyway,
what did it matter? Nor did she believe that drug doses big enough to remove pain
entirely would necessarily cause the patient to develop such a tolerance to the
drug that it would become ineffective. Regrettably many medical institutions and
doctors still hold outmoded views and too many people, suffer unnecessarily if
they are not aware of these issues and are led to believe that there can be no
relief from their pain. Turning again to Jacquie's PSA Rising site, there is an
excellent page on Hospice,
End of Life Care
Dr. Michael Glode's blog also refers to hospice care when he continues:
The
thing that leads to death in most patients, however, is not direct involvement
of an organ like the liver, lungs or brain. Instead, most patients seem to have
a "wasting syndrome" not unlike AIDS. Loss of appetite, loss of energy and general
debilitation lead to weight loss and patients don't feel like getting out of bed.
Hospice care can be extremely helpful for this stage of illness and is usually
available either at home or in an inpatient facility.
The
'wasting syndrome' to which he refers can come from emotional issues like depression
but is usually from Cachexia
or Anorexia (not to be confused with the anorexia nervosa of young women).
If caught early on, anorexia may be treated and weight loss reversed with nutritional
supplements or increased consumption of food. In prostate cancer patients some
molecular causes of cachexia are now known and work is being done to try to address
these, but cachexia does not respond to nutritional supplementation or increased
consumption of food.
One
final point. People who reach this 'end of life' stage will often have fought
against the disease for some time and they, and their doctors, may misjudge how
long they have to live. One
study showed that Doctors who referred terminally ill patients to hospice
care were consistently overoptimistic. In only 20 percent of cases were the doctors'
predictions accurate.
I
hope I have not upset anyone reading this. That was certainly not my intention.
In my life experience our imagination often creates a far worse picture than the
reality that occurs. Knowledge can help rein in the imagination. It may be useful
to listen to an interview with Dr. Pauline Chan, A
Surgeon's Reflections on Mortality or a longer interview (almost one hour)
with her A
surgeon reflects on how Americans face death
The
Four Corners program on Australian Broadcasting Corporation ran a very good program
about palliative care and dying in February 2010 - A
Good Death
Addendum
October 2010: There is a reference to the role of hospice care and its potential
benefits — in terms of quality of life and quality of death in The
"New" Prostate Cancer Infolink which might be of interest.
Addendum
March 2011: Understanding
The Spiritual Needs of the Dying is an excellent article in the Huffington
Post that touches on the question as to whether individuals become more religious
as they die. The author, Kenneth J. Doka Senior Consultant, Hospice
Foundation of America says in part:
"Whether
those who are dying reconnect, review, or renew prior religious beliefs -- or
are even open to new religious experiences -- they are likely to engage in some
form of spiritual searching. That search may be deeply religious or not, but it
is always spiritual, and it can occur whether the person was traditionally religious
or followed another belief system, whether the person was a humanist, atheist,
or agnostic. Despite this reality, spiritual needs of the dying are often overlooked
or ignored by family caregivers, clinicians and even clergy, who may be uncomfortable
with spiritual searching by the dying and with conversations that may occur that
have strong spiritual significance."
This
article is adapted from Living
with Grief®: Spirituality and End-of-Life Care, available from the Hospice
Foundation of America's bookstore. There is a search engine for finding a local
hospice at Senior
Homes - Hospice Care Center.
Addendum
September 2011: Charles (Chuck) Maack
said in a recent post in an Internet Forum:
"While
it saddens all of us when one of our brothers has succumbed to our insidious prostate
cancer, it also brings to mind how fragile are our lives. With this in mind, and
recognizing that too often caregivers/spouses/partners may not have realized the
multitude of home responsibilities that had been carried out by the succumbed
patient, I believe it extremely important for all such caregivers to review and
save the information in the following, since being aware of the considerations
identified and planning well ahead can save one from what could otherwise be an
enormous burden at a time when one is already dealing with the grief of losing
a loved one."
To
this end he has compiled a useful paper covering what he terms End-Of-Life-Considerations.
This is well worth reading and printing out.
Addendum
December 2012:
Most
people approaching the end of their lives have a degree of apprehension about
the possibility of being 'kept alive' whilst suffering pain or in a vegetative
state. It is possible in some jurisdictions to enact a legal document that sets
out clearly the circumstances in which life support is to be terminated, even
if this has fatal results. But there are very few places where people can have
open discussions with their doctors about these issues and put in place legally
reliable instructions. Inevitably whenever this subject comes to the fore it is
clear that changes would be required in legislation. This then leads to a fiery
debate on euthanasia, something which the majority of people in most countries
support in principle.
There
are moves in several States of the United States of America to allow more certainty
in ensuring that the wishes of people are followed. They would be required to
discuss and agree these with their doctor. This process is generally known as
Physician Orders for Life Sustaining Treatment (POLST). Examples of the forms
and details of which States have adopted or are moving towards the acceptance
of these forms are on the POLST
Site.


