A
Primer on Prostate Cancer
Written and Compiled by Donna Pogliano
(Part 1 of 2 parts)

The
Primer which starts below and continues onto the next page has evolved into a
book called "A Primer on Prostate Cancer, The Empowered
Patient's Guide", by Stephen B. Strum, MD, FACP and Donna Pogliano, available
through web booksellers, at local libraries and bookstores and at the website
of the publisher.
(Part
1 of 2 parts)This is a very basic resource for a man and his family if there has been a
finding of elevated PSA (prostate specific antigen) levels in the blood, an abnormal digital
rectal exam, or a recent diagnosis of prostate cancer.
This
is not intended to be medical advice, nor is it intended to replace consultation
with persons in the medical profession. It is intended to be used as a starting
point to increase your knowledge regarding prostate cancer. This primer is not
all-inclusive and new information continues to be available, so your own research
may produce updated data.
If you are leaning toward a specific treatment,
you will need to find specific information regarding the cure rates and possible
side effects both physical and emotional, for that type of treatment. You will
need to consult with your physician to determine if the treatment is appropriate
for your stage and grade of prostate cancer. And you will need to discuss your
diagnosis and your treatment plans with your loved ones.
You
should also be sure to ask your doctor what back-up options are available in the
event the therapy you are considering should fail. And after treatment, you will
need to be vigilant about monitoring your PSA, probably for the rest of your life.
Fortunately, we now have this simple test to monitor the disease and give early
warning if it returns, allowing for more and earlier treatment opportunities.
There is no quick-fix solution to a diagnosis of prostate cancer, and there are
difficulties in finding the fine line between which cancers are "in remission"
and which may be "cured".
This document incorporates the input of a great
many people, all of whom have been touched in some way by prostate cancer. Some
are battling the disease; some are spouses or partners of men who are fighting
prostate cancer. The contributors to this primer are subscribers to various e-mail
discussion groups on prostate cancer. They routinely share their knowledge and
support with others who are feeling bewildered, alone and frightened much the
same as you may be feeling now.
COMMON DENOMINATORS
There
are a few common denominators in all of the contributors' advice to the newly
diagnosed. Those who have "been there, done that" universally recommend that you
move beyond the panic with knowledge, because knowledge is power. And they universally
recommend that you take your time, do your research and arrive at the best treatment
decision for YOU and your family, based on the characteristics of your own health
situation.
Prostate cancer is a "couple's disease." It not only affects
the man, but his sexual partner and his other loved ones. Stress and depression
are common consequences of dealing with the diagnosis, the treatment decision,
the treatment itself, and the side effects of the treatment. If depression becomes
severe and overwhelming, it is appropriate to seek professional help. People deal
with life crises in their own ways. It is especially important during a bout with
prostate cancer to be good to yourself and the people whom you care about and
who care about you, so you are united in the effort to overcome the disease. A
focused, reasoned, and calm attitude will be an asset in dealing with the day-to-day
pressures all of you will face.
Remember-if any treatment really doesn't
feel right, it isn't. If any treatment feels right, it probably is. After you
have studied all your options, trust your instincts along with the knowledge you
have gained. Ask questions until you are satisfied.
Be realistic. If a
man is not generally in good health, surgery may not be the best option. Surgery
of any kind is hard, and recovery is easiest when a person is in good shape. If
a man has bowel or bladder problems already, radiation of any kind may make them
worse. Fortunately, for many patients, there are a number of local treatment options,
including various forms of surgery, radiation therapy or cryosurgery and systemic
hormone therapy or chemotherapies, or a combination of treatments. There are also
treatments under investigation that are not yet approved for treatment of prostate
cancer in the US, but that are being performed elsewhere.
Question your
doctors thoroughly regarding what side effects any treatment you are considering
may produce. Some side effects of treatment are temporary and some become permanent.
There is variation between individuals depending on their physical condition,
age and response to various treatment modalities. There are medications to help
patients cope with bowel or bladder problems resulting from treatment, and a vast
array of measures to cope with partial or even total impotence.
Be aware
that some medical professionals tend to understate risks, and medical professionals
tend to steer you in the direction of their specialty. Urologists tend to favor
the surgical option while radiologists tend to favor radiology. At minimum, you
should have consultations with both, and possibly with an oncologist, a cancer
specialist, who would oversee all aspects of your treatment. Ideally, you should
see a medical oncologist specializing in prostate cancer. Unfortunately, their
numbers are few.
The goal of prostate cancer treatment, it is often said,
is to be sure the patient lives long enough to die of something else. Many prostate
cancers are slow growing. You don't need to make a decision regarding how to deal
with your disease in days or even weeks. Many patients take as long as a few months
to look at their options. You will have time to talk to your family about the
results of your research and discuss the implications of the side effects so you
are sure to be prepared to deal with them, and to be sure you have the support
you need.
CHOOSING A DOCTOR
Choosing a doctor is an important
step toward making a treatment decision. Your choice of treatment and who will
perform it is crucial in giving you the best outcome based on the information
that your test results yield. Your choice of treatment needs to fit with your
age, life expectancy, lifestyle, general health, and your expectations for future
quality of life.
Patient references given by a doctor may direct you to
their successes, not to their failures, so make every effort to verify any information
you are given. This goes for information that doctors give you regarding various
treatment modalities as well. Ask for documentation. Ask other patients who have
been there and done that. Also, realize that the doctor who diagnoses your prostate
cancer may not be the doctor who is your best choice for treatment. Once you decide
on a treatment modality, it is time to search out the experts in that field.
Consider
your priorities. It is not wise either to overtreat your disease based on fear
of recurrence, nor to undertreat your disease based on fear of impotence or other
side effects. Most people would agree that when ordering your priorities, staying
alive is at the top of the list, keeping firmly in mind that dead men don't have
erections either.
If you are uncomfortable with your doctor, switch doctors
until you find one you trust, who will take the time to examine you properly,
answer your questions, and address all of your concerns, physical and emotional.
Be sure to write down your questions in advance of your appointment, so you can
be assured of getting the most out of your consultations.
Take your partner,
wife or a good friend with you to your appointments and consultations. No one
should have to go through this experience alone. Doctors expect to see someone
to act as support, and most are disappointed if a patient arrives at his appointments
alone. Many times, it is that supportive person that researches the options and
questions the doctor. This is perfectly appropriate.
The results of primary
treatment are closely linked to the expertise of the doctor performing the treatment,
so selecting the very best doctor (an artist) for a given procedure will significantly
increase the chance of success. An artist is going to have overall better outcomes
both with eliminating the cancer and with limiting the side effects of treatment
than a mediocre doctor, no matter which treatment modality is your choice. It
is therefore of utmost importance to decide not only on a treatment choice, but
to seek out the best doctor to perform the procedure.
RECORD-KEEPING
Some people tape record every office visit so they can review what
was said later and not be pre-occupied with taking notes. To get the most value
from this approach, it will be necessary to listen to the tape and take notes
about what seems really important.
Be sure to get copies of the results
of all the medical, surgical, diagnostic and therapeutic procedures that are done.
Should you decide to change doctors later, this is valuable information. And you
will need this information, in chronological order, to record items in your prostate
cancer "digest," your own permanent record to be used as a supplement to your
medical records in the event you choose to seek advice regarding your care and
treatment from another source.
Notes regarding conversations with your
doctors, medication and diet changes, anything that may be pertinent to your treatment
should be part of your digest. Doctors who are experts in the field of prostate
cancer volunteer their time on e-mail lists to patients with specific, complex
problems. (See the Resource List later in this primer under "Helplines.") If you
ever wish to use this service, the specifics of your case are most conveniently
communicated by means of your prostate cancer digest. Keep the information in
a safe place.
Seek out experts to perform your treatment. It is not unusual
for patients to travel across the country to seek out the very best medical professionals,
some of whom have performed thousands of successful procedures. These people are
considered "artists." You have a life. You deserve the best treatment.
Many
will accept your insurance company's "reasonable and customary charges" limit
as payment in full, or with only incidental out-of-pocket expense to you. Ask
questions regarding this aspect of your treatment. Some procedures and medications
are very expensive. You need to put your mind at ease up front regarding the financial
burdens you may incur so that you can be free to focus on fighting your disease.
GATHERING INFORMATION
It will be of great benefit in researching
your treatment options and seeking out support if you have e-mail and Internet
access. If you were to put "prostate" into a search engine on the Internet, you
would get more information than you would ever want. We have provided some of
the available Web sites and support group Web sites in the Resource list [at end
of document] for your convenience.
If you don't have computer access,
you might want to visit your local library and see what computer resources they
can offer. Most libraries now have computers for patron use and librarians who
can help you find and print the information you are seeking, so you can read it
later, and have it available for reference. Don't be afraid to ask for help. And
don't be afraid to tell the librarian why you need the information. You may find
that cancer has also touched that person, and they are willing to give compassion
and help. Keeping your diagnosis a secret makes it much more difficult to deal
with.
You have now inadvertently joined the fraternity of prostate cancer.
You have a responsibility to yourself and your loved ones to get the best care
and most information you can. And THEN, to become an advocate for more support
for prostate cancer research, early detection, early cure, and to help mentor
those who come after you as so many others have done. You are in VERY good company!
NUTS AND BOLTS
It is estimated that 50% of men over 50
and 70% of men over 70 have some form of prostate cancer. Some of these cancers
are life threatening, but the majority will grow so slowly as to never be a threat
to life, so more men will die "with" prostate cancer than "of" it. Some men have
such overwhelming health issues before being diagnosed with prostate cancer, that
treatment is not indicated, or that palliative treatment is all that is necessary.
The intention of palliative treatment is to help the patient deal with the pain
and discomfort of the disease and is not intended to cure the disease.
However,
prostate cancer can strike men in their 40's and 50's, and even as young as their
30's, and if life expectancy is more than ten years, more aggressive treatment
is usually indicated. Family history of prostate cancer or breast cancer would
suggest that regular PSA (prostate specific antigen) blood tests be started at
age 35. For other men, screening should begin at age 40.
THE BASICS
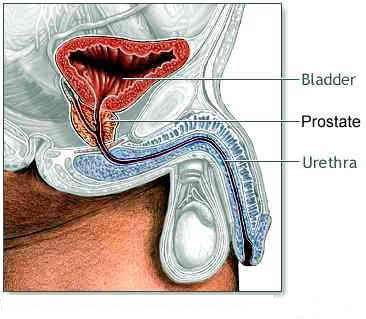 The
prostate gland is part of the endocrine system, a walnut-sized gland that sits
between the bladder and the rectum at the bottom of the pelvis, surrounding the
urethra. It adds vital nutrients and fluid to the sperm, and therefore local treatment
for prostate cancer impacts upon a man's ability to father children. Because local
therapies affect prostatic secretion, they also impact upon a man's sexuality,
specifically affecting the quality of ejaculation and orgasm. Only men have prostate glands.
The
prostate gland is part of the endocrine system, a walnut-sized gland that sits
between the bladder and the rectum at the bottom of the pelvis, surrounding the
urethra. It adds vital nutrients and fluid to the sperm, and therefore local treatment
for prostate cancer impacts upon a man's ability to father children. Because local
therapies affect prostatic secretion, they also impact upon a man's sexuality,
specifically affecting the quality of ejaculation and orgasm. Only men have prostate glands.
Cancer of the prostate gland is not contagious or sexually transmitted. It is generally
accepted that there is a genetic link which increases risk of prostate cancer
and that a diet high in saturated fat over many years can contribute to the development
of prostate cancer.
There is now evidence that there is a hereditary link
between prostate cancer and breast cancer (in women and in men). This genetic
link makes it wise for a man diagnosed with prostate cancer to advise his progeny
of both genders to undertake early and adequate screening for prostate cancer
in his male children and for breast cancer in his female children.
Furthermore,
the younger the blood relative is at the time of diagnosis of prostate cancer,
the greater the risk to his male and female relatives, including children, siblings,
cousins, nieces and nephews. Black men seem to have the highest prostate cancer
incidence, followed by Hispanic men. The causal factors involved could be genetic,
environmental, or a combination of factors and are being investigated. Meanwhile,
it would make sense for men in these groups to be vigilant about PSA testing and
digital rectal exams (DRE's).
HOW DOES CANCER WORK?
Cancer
is a disordered and abnormal cell growth. Cancer cells have lost the ability to
network and communicate in the way that normal cells do, and can no longer function
as intended in the overall framework of bodily chemistry. They also no longer
die as they should, through normal cell death and replacement, and they grow beyond
their normal borders. Eventually, they can overwhelm the system.
Some
cancers are slow growing and not typically life-threatening. Some are aggressive,
fast-growing cancers. There is a lot of variation. Doubling time and velocity
can be calculated by calculated by you or your doctor to determine how fast the
cancer is growing.
Prostate cancer confined within the gland itself is
called "organ confined" prostate cancer. When prostate cancer has not penetrated
the perimeter of the gland, referred to as the prostate "capsule" it is very treatable
with curative intention. Options such as surgery or various forms of radiation
typically result in ten or more years of being disease-free. Some people call
that being in "remission." Most people call that "cured."
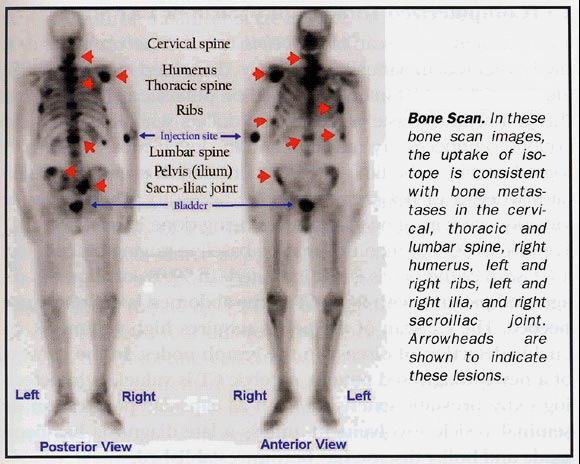
If the cancer
spreads before local treatment can be undertaken, it usually has penetrated the
capsule. After penetrating the capsule, it may spread also to the lymph nodes,
seminal vesicles, adjacent bladder and then to the bone, most often to the spine,
pelvis and ribs. Prostate cancer can also involve vital organs such as liver and
lungs. When it reaches that advanced state, it usually has a fatal outcome.
DIAGNOSIS
AND TESTING
A vast array of testing procedures is available to correctly
assess the character and spread of any particular prostate cancer. Most patients
will not need all the tests that are available, but most doctors will honor an
informed patient's requests for any testing that seems reasonable. Some insurance
companies or HMO's may not agree to pay for all the available tests.
It
is vital that everything that can be known about your cancer be discovered BEFORE
you make a treatment decision. That way, you will have the confidence that the
treatment you undertake will be the best choice of treatment for your particular
situation. Many doctors will stress that with the current available treatment
options, you have ONE chance at a cure if you have organ-confined disease. And
they will not be responsible for making that choice for you, since you need to
live with the consequences of your decision for the rest of your life.
THE
PSA
The first test, used primarily as a screening procedure since
1990, is the PSA blood test. Blood is drawn and tested for the presence of "prostate
specific antigen," a marker in the blood that indicates the presence and extent
of cancer activity. PSA is actually an enzyme made by prostate tissue. Its purpose
is to dissolve the proteins that cause semen to clump. Further investigation to
determine if cancer is present is usually recommended if the PSA is over 4, and
some doctors feel that 2.6 merits monitoring on a six-month basis to see if there
is an upward trend. This will be discussed in more detail below.
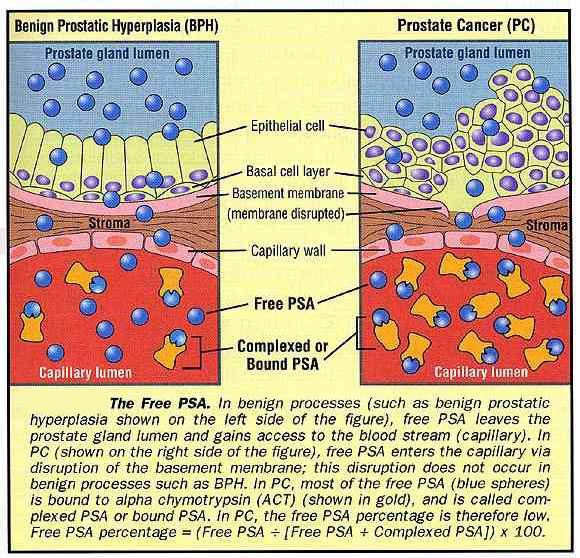
Free
PSA testing can easily be used to weed out some of the patients with PSA's above
4 that are not cancer-related. Free PSA testing (see further information later
in this section) can rule out benign prostate hyperplasia (BPH), but not prostatitis.
At minimum, before
undergoing a biopsy, you should have your PSA tested several times. There is considerable
variation in test results depending on the lab and assay used, so you need several
readings to arrive at an average. Refrain from ejaculation at least 48 hours before
the blood draw, and do not do anything else that massages the gland for one week
prior to the blood draw, such as using a bicycle or exercise bike, or riding a
motorcycle. It is thought that these activities can temporarily raise your PSA,
and could result in unnecessary concern or inappropriate testing based on distorted
PSA results.
Some men with elevated PSA should routinely follow up with
a Free PSA test to help rule out causal factors other than cancer. This is another
type of blood test which might avoid needless biopsies if used more regularly.
However, this test is only reliable for PSA's of between 4 and 10. Recent studies
indicate the lower level of reliability may be 2.5.
Also, after the first
elevated PSA and before a biopsy, some experts recommend that you be tested for
prostatitis, or inflammation of the prostate. If this condition is found, it can
be treated with antibiotics, such as Cipro, usually prescribed for a month or
more. Prostatitis can be a non-cancerous cause of an elevated PSA. Be sure to
wait at least six weeks after the condition is cleared up and medication is discontinued
before rechecking the PSA. Benign Prostate Hyperplasia (BPH) is a result of an
enlargement of the prostate, which also elevates PSA levels. Symptoms can mimic
those found in some cancers, but this is a treatable, non-cancerous condition.
An often-unused approach to PSA evaluation relates to what the PSA levels
are doing over time. Malignant processes relate to persistent cell growth and
production of specific proteins. With prostate cancer, this would relate to PSA
production. If the rate of doubling of the PSA (PSA doubling time or PSADT) or
the rate of increase in PSA (PSA velocity or PSAV) is abnormal, then prostate
cancer is more likely present than not. PSADT should be longer than ten years
to rule in a benign process. PSA velocity should be less than 0.75 ng/ml/year
on the test results to rule out prostate cancer. These are adjunctive tests and
are not absolute criteria for or against malignancy. However, they are valuable
tools and their principles apply to all malignancies.
DIGITAL RECTAL
EXAM
Digital rectal exam (DRE) is used in combination with PSA testing
to determine if there is any evidence of a palpable tumor. The doctor will insert
a gloved finger inside the rectum to feel the gland. This isn't as bad as it sounds.
It may help you to keep in mind that women are routinely poked, pummeled and invaded
in an effort to maintain good health. You can deal with this.
The digital
rectal exam (DRE) will be a factor in establishing the Clinical Stage of your
cancer, which will help to assess your situation and enable you to describe your
condition in a way that others who know what staging means will understand. The
TNM system is used internationally at this time to describe the cancer and it's
spread. "T" describes the tumor, whether or not it can be felt, how large it is
and whether it occupies one or both sides of the prostate. "N" stands for nodes
and describes whether or not the cancer has spread to the lymph nodes. "M" stands
for metastasis, and indicates whether or not the cancer has spread to other organs
or tissues. A full description of TNM staging designations is available on the
Internet. See the Resource List later in this primer under "Quick Reference".
FREE PSA
If PSA is between 4 and 10, requesting a test
for "free PSA" also termed fPSA or PSA II might help to rule out cancer as the
cause. Clarifying the reason for the elevation could spare the patient the intrusion
of a biopsy. This test is a different type of PSA blood test, which can be used
to help rule out non-cancerous enlargement of the prostate gland, called BPH or
benign prostatic hyperplasia. BPH can also cause elevated PSA readings. This test
yields a "% free PSA" number. The lower the number, the more likely you are to
have prostate cancer. A high limit of 25 or more would indicate that the man might
not have cancer. This test should be done routinely if PSA is elevated between
4 and 10, before making a decision regarding undergoing a biopsy.
BIOPSY
OF THE PROSTATE
If a biopsy is done, it should consist of at least
six needle sticks, placed in separate, well-labeled vials so the pathologist can
draw conclusions based on the locations from which the samples were taken. Some
studies indicate that a ten or twelve needle biopsy approach shows an overall
increase in cancer detection of as much as 35% and is recommended.
The
biopsy results will yield the Gleason grades. This is a subjective analysis by
a pathologist of how the prostate cancer appears in the sample (biopsies) as compared
to normal cells. The number will be between 1 and 5 for each Gleason grade, the
higher number indicating a more aggressive cancer. The Gleason "score" or "sum"
will be derived from adding the two grades. The first number indicates the predominant
grade; the second number is the second most predominant grade. The predominant
Gleason grade has to be at least 51% of the total picture seen under the microscope.
The secondary Gleason grade has to be at least 5% of this same picture. This is
stated as, for example, (3,3), which is the most common Gleason score. A Gleason
score of (3,4) indicates that anywhere from 51% to 95% of the specimen is Gleason
grade 3 disease and that anywhere from 5% to 49% of the specimen has a secondary
pattern of Gleason grade 4 disease. Gleason grades 4 and 5 disease are important
NEGATIVE prognostic indicators for the extent of disease and the clinical course
of prostate cancer.
Tissue samples taken during biopsies are preserved
and retained, making it possible to send the samples to an expert prostate cancer
pathologist for review and confirmation. Experts in assessing prostate cancer
biopsies are available at specific labs, such as UroCor, Inc. and Dianon Laboratories,
and at certain major medical centers. Samples from all over the country can be
sent to these artists for "second opinions". Don't be afraid to ask for this additional
assurance that your Gleason is correct, because this will be a MAJOR factor in
your decision-making process. If your Gleason is inaccurate, you may overtreat
or undertreat your cancer based on erroneous information! Refer to the Resource
list [end of document] under "Quick Reference" for a list of expert pathologists
who can be consulted to confirm your Gleason score.
PAP
You
should request a PAP (Prostatic Acid Phosphatase) test after your diagnosis. This
can help determine if the cancer is most likely organ confined or not. This blood
test measures an enzyme in the blood. A PAP of 3.0 or higher is cause for concern.
Since there is no universally accepted standard regarding stated range of PAP
at this time, you should be sure that your test is always sent to the same lab
so that you can be assured of consistent results if you are tracking your PAP
over time.
Persistently elevated levels are considered possible evidence
of metastases (spread of the cancer). It is inconclusive to rule out spread beyond
the capsule, the shell of soft tissue that covers the prostate, because only 75%
of patients with metastases have an elevated PAP. However, if your PAP is 3.0
or higher, most doctors do not consider you a good candidate for surgery, since
the risk of PSA recurrence (PSAR) is four times higher when this level of PAP
is found.
Note that PAP is not particularly useful in predicting local
spread to surgical margins of the gland. But it is one more indicator that may
be useful in predicting which patients are likely to have a relapse after surgery.
If PAP is elevated, hormone therapy may be prescribed to halt or slow the spread
of the cancer. PAP like PSA should not be done for at least five weeks after prostate
biopsies. Ideally, both PSA and PAP should not be done unless 48 hours has elapsed
since any ejaculation.
PROSTASCINT
ProstaScint is a relatively
new technique in which a radioisotope is injected into the bloodstream. The isotope
attaches itself to the cancer, then a gamma-ray camera is used to locate evidence
of cancer, if any, in your body. This test is not 100% accurate, but it can be
valuable in combination with other testing. There are false positives. The ProstaScint
may indicate node involvement, in which case, treatment options would be directed
away from local therapy such as surgery, radiation therapy or cryotherapy.
ProstaScint
is used most often in cases of recurrence of prostate cancer after local treatment
of the gland or in patients with high-risk profiles for non-organ confined prostate
cancer at diagnosis. The patient needs to be made aware that this test uses mouse
antibodies. Some investigational clinical trials exclude anyone who has had a
ProstaScint test for that reason.
ENDORECTAL MRI
Endo-rectal
MRI is a useful tool in establishing evidence of extra-capsular extension, particularly
if it incorporates spectroscopy. This technique is far superior to a routine pelvic
MRI and is associated with a 75% to 90% accuracy rate when there is agreement
between both modalities of imaging. This test is used to help determine the probability
of organ-confined disease. This test is also useful in determining spread to seminal
vesicles and regional nodes. It can also be extremely useful in detecting the
site of prostate cancer in men suspected of having disease but eluding diagnosis
on routine ultrasound guided biopsies.
OTHER TESTS
DNA
ploidy is another test that may be recommended to determine the nature of the
cancer: its aggressiveness and its responsiveness to androgen deprivation therapies.
Ploidy is a term used to describe the chromosome content of the cell population
of a tumor. This would be particularly of interest to patients involved in hormone
therapy to try to determine the likelihood of the effectiveness of the treatment.
Diploid cells have normal chromosome pairs and normal DNA. Diploid cancer cells
tend to grow slowly and respond well to hormone therapy. Aneuploid cells have
abnormal numbers of sets of chromosomes. Aneuploid cancer cells tend not to respond
as well to hormone therapy and to be more aggressive. Aneuploid tumors are more
often associated with high Gleason score prostate cancer (8-10) and non-organ
confined prostate cancer.
Bone scans are often done to determine if there
is any evidence of metastases to the bone, and should routinely be done if confirmed
PSA is over 10. In early stage cancers, this is very rare, so don't panic if your
doctor recommends a bone scan prior to embarking on treatment. It is a precautionary
measure and commonly done. Depending on your PSA and Gleason, your doctor may
even tell you that it is likely it will come back negative or show signs of arthritis,
in which case x-rays may be needed as confirmation. Be sure to tell the doctor
of any past injuries to the bones that may show up as spots on the bone scan.
Your physician may decide to forego a bone scan if your PSA is 10 or less and
your Gleason score, validated by an expert, is 6 or less.
CT scans may or
may not be indicated, depending on the results of other testing.
If the cancer appears to be advanced, this can be one more tool to determine what
your treatment options are. Advanced prostate cancer is usually associated with
high PSA readings of 50 or higher and often Gleason scores of 8-10. CT scanning
is a serious waste of healthcare dollars when used in the workup of 90% of men
with prostate cancer. It is highly insensitive in detecting disease in the lymph
nodes and valueless in most patients in detecting extra-prostatic extension such
as capsular penetration or seminal vesicle involvement. In the setting of high
PSA and/or high Gleason scores, a CT scan may disclose lymph nodes that are greater
than 1.0 centimeters in diameter. When such nodes are found they are associated
with a specificity for prostate cancer of almost 100%.
CGA testing measures
the blood levels of Chromogranin A. This test is used to help identify patients
with an aggressive form of prostate cancer and to help track their response to
treatment. In such patients, the CGA elevation should be shown to be progressive
and not just sporadically elevated. CGA elevations in conjunction with elevations
in other markers such as NSE (Neuron-Specific Enolase) or CEA (CarcinoEmbryonic
Agent) are cause for serious concern of mutated aggressive prostate cancer. Always
put these findings in context with the rest of the clinical and pathological picture.
After the results of testing have been obtained, and prior to a treatment
decision, you and your doctor should consult the Partin Tables to determine the
probability of organ-confined disease, probability of spread to the seminal vesicles,
and probability of lymph node involvement. See further discussion of the Partin
tables in the section of this primer under Radiation Therapy, Permanent Seed Implants.
More information on Markers and Tests for Prostate Cancer is available
on the Internet. See the Resource List later in this primer under "Quick Reference".
(Go
to page 2 which starts with TREATMENT OPTIONS)
You
may print one copy of A Primer on Prostate Cancer for your own personal use. The
entire document is available for easy printing as a Word.doc
file (98 KB) or in Adobe.pdf (150 KB)
Copyright
Donna Pogliano © 2000. All rights reserved.